Bright Light Therapy (BLT) corrects circadian rhythm phase delay. BLT treatment in the morning shifts the circadian rhythm earlier, which leads to less discordance between the circadian rhythm and the actual clock time. This helps treating seasonal affective disorder (SAD).
Introduction to Bright Light Therapy
In the pioneering study on SAD (see below) in 1984, Rosenthal and his colleagues used bright white light to mitigate seasonal affective disorder symptoms. They used white full-spectrum fluorescent light (2,500 lux) for 3 hours at dawn (the time of morning when the Sun is 6° below the horizon) and hours at dusk for two weeks.
Now, almost four decades with Bright Light Therapy (BLT) protocol for treating SAD has been optimized. The current recommended protocol is outlined in the table below.
|
Parameter |
Description |
|
Light source |
Fluorescent light box with diffusion screen |
|
Illuminance (lux) |
|
|
Light wavelengths |
Full-spectrum visible light (400–700 nm) |
|
Light source position |
|
|
Daily treatment length |
Morning treatment with time varying depending on the illuminance of light (i.e. 30 mins for 10,000 lux, 1–2h for 2,500 lux). |
|
Treatment duration |
|
|
Treatment variations |
|
|
Possible side effects |
|
Table: Initial parameters for BLT.
Source: Adapted from: Campbell, P. D., Miller, A. M., & Woesner, M. E. (2017). Bright light therapy: seasonal affective disorder and beyond. The Einstein Journal of Biology and Medicine 32: E13–E25.
Two meta-analyses of randomized blinded and controlled studies consistently demonstrate and confirm that BLT is effective in the treatment of SAD when compared to a control. Bright Light Therapy is also widely accepted and considered the primary treatment of Seasonal Affective Disorder (see below).
Seasonal Affective Disorder (SAD)
Seasonal Affective Disorder (SAD) was first discovered and defined in 1984. In a pioneering study, Rosenthal and his colleagues investigated 29 patients who lived in a temperate climate, such as the Nordic countries, with long, dark and cold winters. They experienced depressive episodes specified with weight gain, hypersomnia, overeating and carbohydrate craving during the winter time.
After this pioneering study, a few years later SAD was added into DSM-III (DIagnostic and Statistical Manual of Mental Disorders) as a diagnosis. Lately, SAD has been officially referred to as Major Depressive Disorder (MDD) with a Seasonal Pattern.
Other typical symptoms of SAD include losing interest in activities you once enjoyed, having low energy and feeling sluggish and having difficulty concentrating. Characteristics are also that symptoms go into remission by the spring or summer at the latest.
At present, SAD is defined as recurrent episodes of major depression meeting the following criteria (DSM-V):
- At least two consecutive years where the onset and offset of depressive symptoms occur at characteristic times with no non-seasonal episodes
- A temporal relationship between onset of symptoms and time of year
- A temporal relationship between remission of symptoms and time of year
- An outnumbering of seasonal compared to non-seasonal episodes throughout the lifetime of the patient
SAD may also appear in another form, which is known as the summer-pattern SAD. The symptoms for that include:
- Trouble sleeping (insomnia)
- Poor appetite, leading to weight loss
- Restlessness and agitation
- Anxiety
- Episodes of violent behavior
Because sunlight is the key to SAD, it is rationalized that cases that occur during the summer months may result from too much sunlight exposure. Too much sunlight turns off melatonin production. Also, when the light period of the day is very long (e.g. almost 20 hours in the midsummer in Finland), melatonin production is significantly reduced compared to winter time. Usually, people living closer to the equator get summer-onset SAD.
Even until today, the exact pathophysiological mechanisms of SAD are not fully established or clear. The most popular hypothesis to SAD was that shorter days in the winter with longer duration of nocturnal melatonin secretion leads to depressive symptoms in genetically susceptible individuals.
Today two proposed mechanisms together may explain SAD at the physiological level. The first one hovers around circadian rhythm disruption. It is called the phase-shift hypothesis, which postulates an optimal relationship in the alignment of the sleep-wake cycle and the endogenous circadian rhythm. Based on this theory, the phase delay is causing the symptoms of SAD.
The second proposed mechanism is based on serotonin levels. It appears that in control individuals, when compared to individuals with SAD, there is a better binding potential at the presynaptic serotonin transporters during the fall and winter. This hypothesis explains that if better binding at the transporter results in greater uptake of serotonin into the presynaptic neuron and less available serotonin in the synapse cleft, the outcome could be the appearance of depressive symptoms in affected individuals.
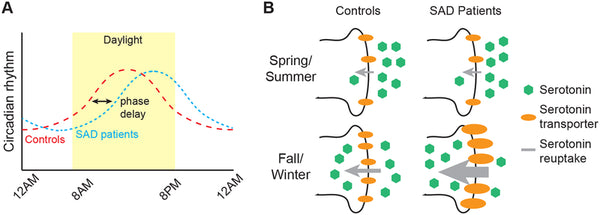
Image: Proposed mechanisms of Seasonal Affective Disorder.
Source: Campbell, P. D., Miller, A. M., & Woesner, M. E. (2017). Bright light therapy: seasonal affective disorder and beyond. The Einstein Journal of Biology and Medicine 32: E13–E25.
BLT mechanisms of action
- BLT corrects circadian rhythm phase delay. BLT treatment in the morning shifts the circadian rhythm earlier, which leads to less discordance between the circadian rhythm and the actual clock time.
- BLT increases available serotonin in the synaptic cleft. BLT treatment during fall and winter reduces the serotonin transporter binding potential, which can lead to less uptake thus leading to greater amount of available serotonin.
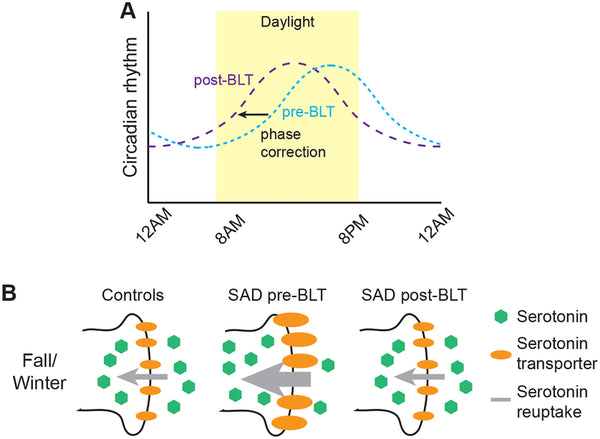
Image: Mechanisms of BLT action based on proposed pathophysiology of Seasonal Affective Disorder.
Source: Campbell, P. D., Miller, A. M., & Woesner, M. E. (2017). Bright light therapy: seasonal affective disorder and beyond. The Einstein Journal of Biology and Medicine 32: E13–E25.
Other mechanisms include enhancing alertness and optimizing sleep homeostasis by increasing EEG delta activity and sleep pressure. BLT also seems to modulate monoaminergic pathways (mainly dopamine).
Biohack your performance & mood with light-therapy glasses
Propeaq light therapy is based on scientific studies regarding the balance between performance and sleep. The Dutch company Propeaq has taken the insights around the right conditions for creating balance and have developed this patented product.
Propeaq’s blue light has a wavelength of 468 nanometers at an intensity of only 35 lux. The LEDs are just over half an inch (1.5cm) from the eyes and are harmless for normal use.
More than 450 Olympic athletes from 11 countries are using PROPEAQ light glasses. Use blue lens together with blue light when you need energy and change it to red lens before bed to block the blue light from outside to promote melatonin production and improve your sleep.
CHECK OUT PROPEAQ GLASSES HERE.
In the Resilient Being Book we dive deep into measuring circadian rhythms with various scientifically validated methods. Finding your biological chronotype is also crucial for optimizing circadian rhythm patterns with light exposure.
///
Do you suffer from SAD? Have you tried BLT? Tell us in the comments.
This article is an excerpt of our forth-coming massive sequel to Biohacker's Handbook, called the Resilient Being. You can pre-order it here!






