Silent inflammation lurks behind almost all diseases. In this article, you will learn what silent inflammation is and how it can be controlled by lifestyle. Diet, nutritional supplements, and other lifestyles significantly affect it.
INTRODUCTION
Inflammation and its activation, as well as the entire inflammatory system in general, are an important part of the body’s internal defense system. In the inflammatory process, the immune system recognizes and removes the harmful stimulus, after which the healing process begins.
Inflammation can be roughly divided into acute and chronic (silent) phases. An acute inflammatory condition is usually caused by an external microbe, trauma, toxic substance, or other similar factors. Chronic inflammatory disease, on the other hand, develops over a long time (usually lasting several years) in a situation where the normal self-regulatory process (resoleomics) of acute inflammation and its cessation are disrupted.
The acute inflammatory process involves three phases:
- Initiation phase (start)
- Resolution phase (middle)
- Termination phase (end)
This process is also substantially influenced by the sympathetic nervous system and the HPA axis that regulates stress responses. This means that constant chronic stress and overactivity of the HPA axis and the sympathetic nervous system (“fight or flight”) can disrupt the above-mentioned inflammatory process and cause a chronic inflammatory condition. This process leading to a chronic inflammatory state is facilitated by insulin resistance (decreased sensitivity of cells to insulin) and cortisol resistance (decreased sensitivity of cells to cortisol). These two resistances often go hand in hand.
Researchers have also found in modeling this process that non-steroidal anti-inflammatory drugs (NSAIDs), which are often used to treat inflammation and pain, interfere with the normal inflammatory process. They can also prevent the body from recovering normally and, in fact, contribute to the development of a quiet inflammatory state. NSAIDs interfere with this process, especially in the context of chronic stress.
The normal termination of the inflammatory process is disturbed, in particular, due to the following factors:
- Antioxidants and other anti-inflammatory molecules are not available.
- Pro-inflammatory (inflammatory) molecules are constantly overproduced, and the eicosanoid switch does not turn on (see illustration on next page).
- There is a constant excess of noradrenaline in the body, the relative amount of which exceeds the amount of cortisol.
- Inflammation stops when more cortisol is produced than norepinephrine (see picture).
Prolonged (silent inflammation) can be caused by factors such as:
- Failure to eliminate acute microbial inflammation, which can lead to chronic infection
- Continuous low-level exposure to environmental toxins that the body cannot effectively eliminate
- An autoimmune disease in which the body attacks itself
- Recurrent acute inflammatory conditions that may become chronic
- Persistent inflammatory condition caused by free oxygen radicals, AGEs (advanced glycation end-products), uric acid, oxidized lipoproteins, oxidative stress, and mitochondrial dysfunction (very common condition), etc.
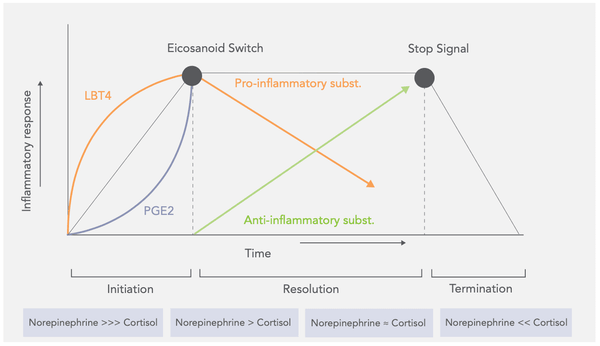
Image: INFLAMMATION IS A CONTROLLED THREE-PHASE PROCESS REGULATED BY THE SYMPATHETIC NERVOUS SYSTEM AND THE HPA AXIS
Diseases caused by chronic (silent) inflammation include cardiovascular disease (CVD), diabetes, arthritis and other joint diseases, chronic kidney disease, allergic asthma, inflammatory bowel disease, and chronic obstructive pulmonary disease or COPD. Chronic inflammation is also known to be a significant factor in the development of cancer.
Risk factors for silent chronic inflammation include:
- Aging
- Obesity (and metabolic syndrome)
-
Diet (a diet that generally increases inflammation, see
- information later)
- Smoking
- Low levels of sex hormones (testosterone, estrogen)
- Stress (especially chronic)
-
Difficulty sleeping and too little sleep
- Symptoms associated with silent chronic inflammation include:
- Pain in the body
- Persistent exhaustion and insomnia
- Depression, anxiety, and mood swings
-
Intestinal symptoms such as constipation, diarrhea, and
heartburn/dyspepsia - Weight gain
- Persistent illness and infections
- Serum protein electrophoresis (SPE) measuring blood globulins
- Used mainly in hospitals; chronic in the diagnosis of diseases
- High-sensitivity C-reactive protein (hs-CRP)
- The cheapest and most used marker
- Acute infection and inflammatory condition also increase the value
- Fibrinogen
- Rises in connection with acute phase reactions
- For example, high fibrinogen is a coronary heart dis- ease independent risk factor
- Pro-inflammatory cytokines such as TNF-alpha, IL1- beta, IL-6 and IL-8
- Expensive to measure but specific to different inflammatory premises in the body
Of the laboratory markers mentioned above, high-sensitivity CRP is by far the easiest to measure and provides a clear picture of the body’s silent inflammatory level.
HIGH-SENSITIVITY C-REACTIVE PROTEIN (HS-CRP)
The levels of C-reactive protein (CRP) in the blood increase during inflammation or infection, as well as cardiac arrest, surgery, or trauma. C-reactive protein is formed throughout the body, especially in the immune system cells, the liver, and fat cells. By binding to other molecules, CRP participates in the production of cytokines and other inflammatory agents.
High-sensitivity C-reactive protein (hs-CRP) is an excellent marker for determining low-level inflammation (or “silent inflammation”). It plays a significant role in atherosclerosis and other inflammatory diseases. Elevated silent inflammation is also a contributing factor to practically all degenerative diseases.
NB! CRP may become elevated due to acute illness, tissue trauma, or infection (usually significantly higher than 10). It should not be used for risk assessment of cardiac diseases under these circumstances. Prolonged, very strenuous exercise may also cause slightly elevated CRP.
Elevated high-sensitivity CRP is an independent risk factor for mortality involving cardiovascular diseases in particular. A comprehensive meta-analysis published in 2017 found that the overall mortality risk of individuals with the highest hs-CRP levels was more than 75% higher compared to the group with the lowest hs-CRP levels. Individuals of the high hs-CRP group had 2.03 times the risk of dying of cardiovascular diseases than individuals with low hs-CRP levels. Increased high-sensitivity CRP levels are linked to cancer mortality in men. This link was not found in women.
The Molisani study published in 2016 (an Italian population of 20,377 adults) found that the individuals with hs-CRP levels in the bottom quarter (0.72 mg/L) had a significantly lower mortality rate compared to the individuals with hs-CRP levels in the top quarter (2.75 mg/L).
Another comprehensive meta-analysis published in the same year studied the effect of the dietary inflammatory index on equivalent variables (overall mortality, cardiovascular disease mortality, and cancer mortality) in a European population. A link was found between the dietary inflammatory index (DII) and all the above-mentioned variables. In other words, the more inflammatory the diet, the higher the levels of silent inflammation in the body, as well as mortality. As such, consuming an anti-inflammatory diet (see below) appears to be one of the clearest dietary factors for health and longevity.
A 2009 review found an inversely proportional link between DII and hs-CRP – the higher the DII (anti-inflammatory potential), the lower the hs-CRP. Body mass index (BMI) has also been found to correlate with hs-CRP (obesity linked with high hs-CRP).
Some DII definitions use a negative value for anti-inflammatory foods, i.e. the lower the DII, the more effective the anti-inflammatory potential. Conversely, the higher the DII, the greater the inflammatory potential of the food.
All studies involving the dietary inflammatory index and silent inflammation have found one common denominator: the typical Western diet. This diet relies heavily on the consumption of inflammatory foods such as processed cereal, dairy, and meat products, white sugar, and refined carbohydrates. The general finding has also been that the typical Mediterranean diet is associated with reduced silent inflammation. This diet relies heavily on the consumption of extra virgin olive oil (EVOO), fish and seafood, vegetables, berries, fruits, and unprocessed whole grain cereals (see a more detailed list below).
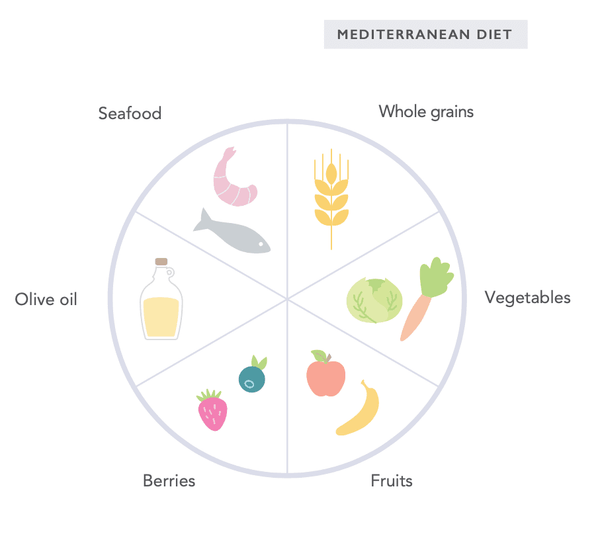
- Extra virgin olive oil (EVOO)
- Foods rich in omega-3 fatty acids, such as fish and seafood
- Turmeric
- Ginger
- Rosemary
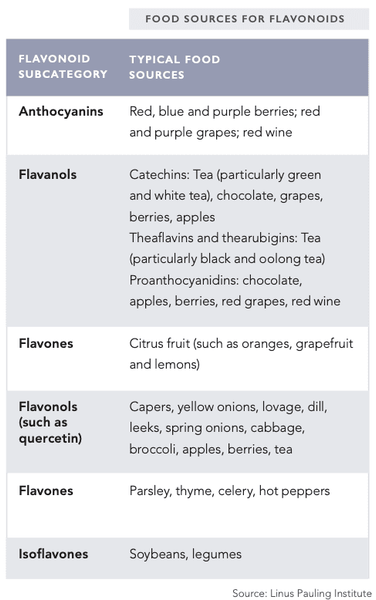
- Polyphenols (incl. flavanols, flavonoids, anthocyanins, isoflavones, etc.)
- Local berries (the darker the better, the wilder the better)
- Green tea, black tea, coffee
- Dark chocolate
- Apples and citrus fruits
- Onions and cabbages
- Spices such as dill, lovage, thyme, parsley, peppers, and paprika
- Legumes
- Capers
- Red grapes and red wine (be mindful of portion sizes – excessive portions increase inflammation)
- Celery
- Foods containing carotenoids
- Carrot, sweet potato, spirulina, chlorella, kale and other dark green vegetables, seaweed, celery, rosehip
- Lycopene (such as in tomatoes)
- Garlic
- Fiber (both soluble and insoluble)
Vitamins and minerals that reduce silent inflammation include:
- Vitamin D
- Vitamin C
- Vitamin E
- Zinc
- Magnesium
- Vitamin A
- Vitamin B6
- Selenium
- Niacin (vitamin B3)
- Folate (vitamin B9)
Ideally, the intake of these vitamins and minerals should be guaranteed from nutrition; however, sometimes dietary supplements are necessary if the diet does not provide the amounts required for optimal intake.
- White sugar and carbohydrate-rich foods (particularly processed and refined carbohydrates)
- Processed vegetable oils and the excessive intake of omega-6 fatty acids
- Trans fats (such as margarine and “junk food”) Processed dairy products (particularly low-fat and highly
- refined products)
- Processed meat products
- Processed cereal products
- Alcohol (excessive use)
- Processed soy products
- Artificial sweeteners, diet soda
- Excessive saturated fat from processed foods
- Stress management such as breathing exercises, meditation, mindfulness, etc.
- Balanced physical activity (excessive stress increases inflammation, as does a sedentary lifestyle [approx. 9 MET-hours / week, i.e. as per official guidelines])
- Normal body weight
- Avoiding chemicals and toxins found in the environment, as well as removing these from the body Sufficient and high-quality sleep
- Balanced blood sugar levels
- Psychological and emotional balance
- Regular fasting and/or intermittent fasting
REFERENCE RANGES (HS-CRP)
These values are determined based on the risk of cardiovascular disease:
- Less than 1.0 mg/L = low (relative) risk
- 1.0–3.0 mg/L = medium (relative) risk
-
More than 3.0 mg/L = high (relative) risk
Get these 3 incredible products to manage silent inflammation!
Magnesium:https://shop.biohackercenter.com/products/elsavieredfiber?_pos=1&_sid=52a3b259e&_ss=r
Elsavie exclusive fiber blend with turmeric:https://shop.biohackercenter.com/products/elsavieredfiber?_pos=1&_sid=52a3b259e&_ss=r
Primeadine:https://shop.biohackercenter.com/products/primeadine?_pos=3&_sid=edc2f7291&_ss=r





