Does high cholesterol cause heart disease and atherosclerosis? Do you need to avoid butter, and what about saturated fat? All about cholesterol in this article. Also order Biohacker's Cholesterol guide!
INTRODUCTION
Cholesterol is probably one of the most controversial, if not the most controversial, topics related to nutrition, medication, and general well-being. Cholesterol-lowering drugs are used more than ever, eggs are still being avoided because of the cholesterol they contain, and high cholesterol has become a detrimental factor over time. This interpretation has luckily been challenged in the past decade, and more extensive research data on cholesterol concerning heredity has become more prominent. Cholesterol in eggs or other foods isn’t actually harmful, saturated “hard fat” does not clog arteries, artificially lowering cholesterol with drugs may not always be a good thing, and the side effects of cholesterol drugs have also begun to be better understood.
CHOLESTEROL
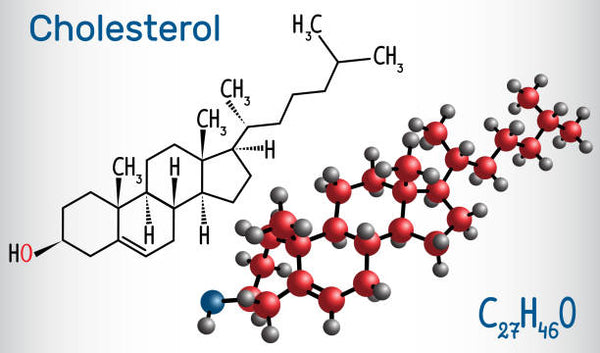
Cholesterol is structurally steroid alcohol (sterol). The body is capable of producing cholesterol independently in all tissues; however, it is predominantly produced in the liver. Cholesterol is also found naturally in animal-based foods. Cholesterol forms a vital part of the cellular membrane where it maintains both structural balance and elasticity (approx. 30% of the entire cellular membrane). Unlike plants, animal cells can function without cell walls thanks to cholesterol. Cholesterol is necessary for the biosynthesis of steroid hormones, bile acid production, and vitamin D synthesis.
An individual synthesizes approximately 1,000 mg of cholesterol per day. There is approximately 35 g of cholesterol stored in the body. Adult Finnish men receive on average 296 mg of cholesterol per day from food; for adult women, it is 210 mg per day. In the US, the mean dietary cholesterol intake was 293 mg/day (348 mg/day for men and 242 mg/day for women) based on the 2013–2014 survey cycle. Previously, the Dietary Guidelines for Americans recommended that cholesterol intake be limited to no more than 300 milligrams per day. The 2015 DGAC (Dietary Guidelines Advisory Committee) will not bring forward this recommendation because available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol, consistent with the conclusions of the AHA/ACC report. Cholesterol is not a nutrient of concern for overconsumption. This is due to significant genetic variation in the absorption of cholesterol and thus the resulting changes in blood cholesterol levels.
The most cholesterol-rich food is the egg. Many people continue to avoid frequent egg consumption, despite the fact that the link with increased risk of coronary artery disease and cardiac mortality has been refuted in all recent studies and meta-analyses. The studies conducted have not found a strong correlation between egg consumption and increased cholesterol levels.
HIGH CHOLESTEROL AND ATHEROSCLEROSIS: IS THERE A CAUSAL RELATIONSHIP?
Elevated cholesterol is not a problem in and of itself ; however, physiological problems occur more frequently when elevated cholesterol is combined with elevated silent inflammation, insulin resistance, and endothelial damage, as well as a high number of low-density lipoprotein (LDL) particles (NB! Not LDL cholesterol). A link has also been found between this and metabolic syndrome.
Elevated cholesterol levels caused by inflammation and endothelial damage to the inner wall of blood vessels may lead to a build-up of LDL particles in the blood vessels (glycoprotein webs) and impair the blood flow to the heart, brain, and other organs. Studies have shown that the condition behind atherosclerosis (the build-up of plaque in the arteries) is indeed subendothelial lipoprotein retention. In plain English, this refers to lipoproteins building up at sites of inflammation and thickening the blood vessel walls, thereby reducing the lumen (space) inside the blood vessel. The anti-inflammatory diet can help prevent this change.
On the other hand, theories have been proposed suggesting that LDL particles in and of themselves are harmful “foreign objects” that, upon sticking to the artery glycoprotein web, cause inflammation. The situation only becomes a real problem when the inflammatory reaction becomes prolonged and chronic – building up atherosclerotic plaque that in turn forms cholesterol crystals.
Endothelial damage and inflammation can be affected by several factors such as:
- Chronic infections, such as H. pylori and Chlamydia pneumoniae
-
The microbial balance of the intestines and/or abnormal
intestinal permeability (causes endotoxemia) - Metabolic disorders
- Environmental toxins (especially heavy metals)
- Hypothyroidism
-
Genetic factors
FAMILIAL HYPERCHOLESTEROLEMIA
Familial (genetic) hypercholesterolemia (FH), or high cholesterol levels, must be treated to reduce the risk of cardiovascular disease. This is commonly done with medication, although dietary and lifestyle treatment can also be helpful.
The latest (2017) comprehensive international meta-analysis found that familial hypercholesterolemia occurs in 1 in 250 individuals. In Finland, for example, the frequency is 1 in 500, although the most recent comprehensive Finnish review (2015) suggests that FH is underdiagnosed in Finland. The US prevalence of probable/definite FH was estimated to be 0.40% or 1 in 250. This suggests that 834,500 US adults have familial hypercholesterolemia.
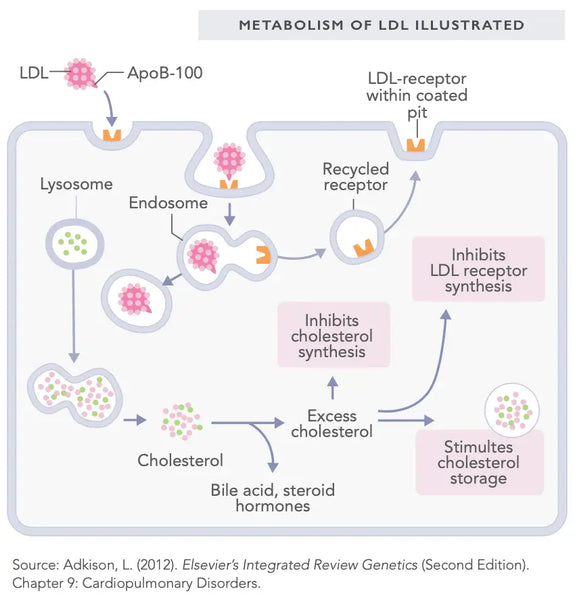
Familial hypercholesterolemia occurs in either heterozygote or homozygote form. The first is significantly more common – it means the individual inherited a faulty gene from only one parent while the other allele functions normally. FH involves a mutation in the LDL receptor-coding gene or the apolipoprotein-B (ApoB) coding gene. Some other mutations have also been found, but these are extremely rare.
The LDL receptor is located on the cell membrane where LDL particles attach to it. Conversely, ApoB is part of the LDL particle that binds to the LDL receptor. A lock and key analogy may help understand their relationship: ApoB is the key and the LDL receptor is the lock – both must work well for LDL cholesterol to transport the LDL particles into the cells and out of the blood circulation. When this is dis- rupted, the amount of LDL particles in the blood increases significantly. The particle-carrying LDL cholesterol usually also increases, although these are not directly proportional.
NB! Familial hypercholesterolemia is diagnosed with a combination of clinical picture and laboratory tests. Interpretation always requires the expertise of a medical doctor. Typically, total cholesterol is at 10 mmol/L (with a range of 8–15 mmol/L).
TOTAL CHOLESTEROL (TC)
Factors that increase total cholesterol include smoking, excessive and ongoing alcohol use, untreated hypothyroidism, diabetes, obesity, menopause, low level of physical activity, and genetic factors. High-fat diets (such as ketogenic or low-carb diets) may also temporarily increase total cholesterol levels; however, the effect is usually temporary. Hypothyroidism should always be ruled out if the total cholesterol levels are significantly elevated.
Low total cholesterol may cause vitamin D deficiency, steroid hormone production problems, depression, and an increased risk of premature death from various causes.
Thyroid hormones stimulate the production of LDL receptors in the liver. Sex hormone-binding globulin (SHBG, see Section 4) binds LDL cholesterol, thus reducing the levels of LDL cholesterol in the blood. With hypothyroidism, the amount of LDL receptors produced is insufficient, leaving more LDL cholesterol in the blood. This raises LDL cholesterol levels as well as total cholesterol.
The activity of the LDL receptor is also influenced by insulin, the effect of which is carried by PCSK9. PCSK9 binds to apolipoprotein B100 on the surface of LDL particles, which prevents these from binding to LDL receptors, thus blocking their entry into the cells. The better and more stable the regulation of insulin secretion and insulin sensitivity, the better the functionality of cholesterol metabolism through PCSK9 inhibition.
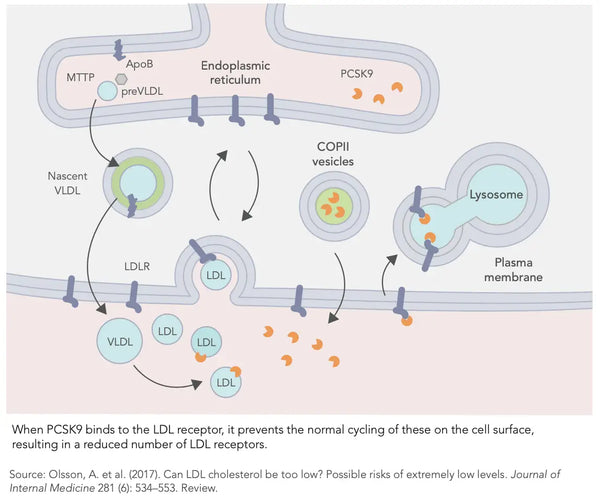
Another factor regulating the occurrence of PCSK9 is inflammation – the more severe the inflammation, the higher the level of PCSK9, which in turn significantly increases the level of cholesterol in the blood. Conversely, a lower level of PCSK9 is associated with reduced inflammation. High PCSK9 levels are also linked to the build-up of atherosclerotic plaque (associated with coronary artery disease).
In 2004, the Nordic Reference Interval Project (NORIP) determined the reference range for total cholesterol for healthy adults:
The reference range for adults according to the NORIP study are:
- Aged 18–29: 2.9–6.1 mmol/L or 112–236 mg/dL
- Aged 30–49: 3.3–6.9 mmol/L or 128–267 mg/dL
-
Aged 50+: 3.9–7.8 mmol/L or 151–302 mg/dL
Similarly, a population survey of nearly half a million people, including South Korean men (30–65 years), published in 2000, found that the lowest mortality was when total cholesterol was 5.5–6.5 mmol/l (or 211 to 251 mg/dL). A similar conclusion was reached in a follow-up study published in 2019 including 12.8 million adults. In addition, it was found that too low cholesterol was associated with higher overall mortality compared to too high cholesterol.
A study conducted on elderly people who were admitted into hospital care found that the highest level of mortality involved individuals with the lowest total cholesterol levels (less than 4.14 mmol/L). An inversely proportional link was found between mortality and cholesterol levels – the lower the levels, the higher the mortality. A Swedish study published in 1997 indicates that a low total cholesterol level (less than 4.7 mmol/L) is linked to higher frequency of depression in middle-aged women.
NB! This article does not take a stance on the use of cholesterol medication. The use or disuse of medication should be discussed with your primary physician.
P.S. In the next article, we will discuss HDL and LDL cholesterol and how you can optimize your cholesterol levels through your lifestyle.





