This article covers HDL and LDL cholesterols and their optimization with lifestyle including diet, nutrition, exercise, supplements and other interventions. If you want to get a comprehensive picture of cholesterol as a topic with its markers and want to understand how silent inflammation and insulin sensitivity also affect the development of possible cardiovascular disease, get Biohacker's Cholesterol Guide.
HDL CHOLESTEROL
High-density lipoprotein (HDL) cholesterol is a group of lipoproteins that carry cholesterol around the body. HDL cholesterol consists mostly of protein with a small amount of cholesterol. Approximately 20% of the serum cholesterol is bound to HDL. HDL is considered the “good” cholesterol because it removes excess cholesterol from the blood and transports it back to the liver for destroying or recycling. Both LDL cholesterol and HDL cholesterol are vital for optimal cholesterol transportation. Elevated HDL cholesterol levels in the blood are often linked to plaque build-up in the minor blood vessels, reducing the risk of cardiac arrest or stroke.
Low levels of HDL cholesterol are commonly found in association with:
- coronary artery disease
- type 2 diabetes
- uremia
- hypertriglyceridemia
- menopause50
A sedentary lifestyle, smoking, and obesity reduce HDL levels.
Factors that increase HDL cholesterol include:
- high-quality fat (such as extra virgin olive oil) consumption
- exercise
- a low-carbohydrate diet including
- In terms of carbohydrate intake, sugar, in particular, has been linked to low HDL cholesterol levels
- fish
- polyphenols
- fibers
- omega-3 fatty acids.
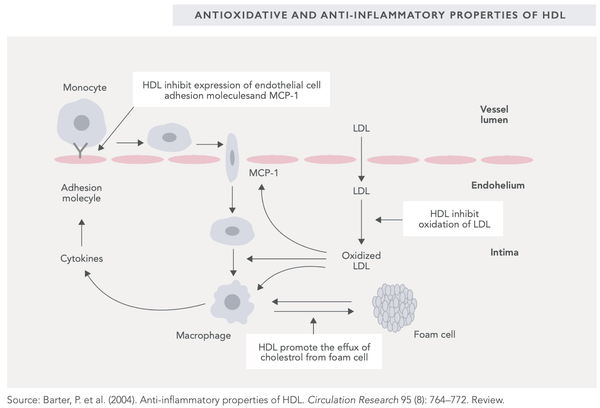
HDL cholesterol indicates how much cholesterol is bound to HDL proteins. HDL cholesterol has been found to have anti-inflammatory effects in the body due to its ability to regulate macrophages. These anti-inflammatory and antioxidative effects (inhibiting LDL oxidation) help explain HDL’s ability to protect the body from atherosclerosis (see image). Ideally then, HDL cholesterol levels should be sufficiently high enough to achieve the aforementioned effects.
However, high levels of HDL cholesterol do not automatically indicate a lower risk of cardiovascular disease. This, as do many other things, depends in part on genetic factors. The endothelial lipase gene (LIPG) variant Asn396Ser carriers have high cholesterol levels, but no elevated risk of cardiac events such as heart attacks has been detected. Conversely, approximately 10% of cases of low HDL cholesterol levels can be attributed to a genetic mutation in genes APOA1, ABCA1, or LCAT.
LDL CHOLESTEROL
Low-density lipoprotein (LDL) cholesterol is a lipoprotein that carries cholesterol (70% of all cholesterol) in the blood. LDL cholesterol consists mostly of cholesterol and a small amount of protein. It is the primary cholesterol-carrying lipoprotein in the blood. LDL cholesterol carries LDL particles, meaning that LDL cholesterol acts as a transportation for them. Cells receive LDL particles and utilize the lipids needed. LDL cholesterol moves relatively slowly in the blood and is therefore prone to oxidation (ox-LDL). Oxidized LDL that attaches to the endothelium significantly impairs blood vessel function and circulation (read more about oxidized cholesterol from the Biohacker's Cholesterol Guide).
High LDL and total cholesterol levels, when occurring together with inflammation or endothelial damage, may lead to the build-up of atherosclerotic plaque and the resulting constriction of blood vessels, cardiovascular disease, and later cardiac arrest and stroke.
The likelihood that cholesterol from LDL particles will migrate to the arterial walls depends predominantly on the number of particles. The larger the number of LDL particles entering the artery wall, the more they are oxidized, and eventually the macrophage foam cells absorb cholesterol into the walls of the arteries, creating hardening or plaques.
This is why LDL cholesterol is often called “bad” cholesterol. Epidemiological studies have found that in healthy individuals, LDL cholesterol is linked to increased arterial plaque and higher overall mortality. However, a cause-and-effect relationship should not be interpreted from these findings.
It appears that prolonged high LDL cholesterol levels have a cumulatively detrimental effect, increasing the hardening of arteries. Individuals with a high risk of cardiovascular disease benefit from lowering their LDL cholesterol levels (particularly individuals with familial hypercholesterolemia).
NB! Low LDL cholesterol levels (including total cholesterol) do not guarantee that atherosclerosis will not develop. This has been found in several studies tracking the relationship between cardiac mortality and LDL cholesterol levels. In some cases, low LDL cholesterol levels have even been linked to higher cardiac mortality. For this reason, as well, the primary concern should be the good management of silent inflammation and insulin sensitivity in order to inhibit the development of cardiovascular diseases.
Excessively low LDL cholesterol levels may lead to various health issues such as:
- disruptions in the production of steroid hormones and bile acids
- disruptions in adrenal gland function
- depression
- type 2 diabetes (complication caused by statins)
- anxiety
- neurological problems
- self-destructiveness
- stroke
Factors that increase LDL cholesterol include:
- smoking
- excessive alcohol use
- poor diet (low on vegetables and good fats)
- obesity
- sedentary lifestyle
A high-fat diet (such as a ketogenic or low-carb diet) may also temporarily increase LDL cholesterol levels (see above), although after an adaptation period of a few months they usually return to a level that is lower than before.
According to a very recent study (2021) published in The American Journal of Clinical Nutrition, the authors propose a novel model (the homeoviscous adaptation to dietary lipids (HADL) model). It explains changes in lipoprotein cholesterol as adaptive homeostatic adjustments that serve to maintain cell membrane fluidity and hence optimal cell function. The authors propose that circulating lipoproteins serve as a buffer to enable the rapid redistribution of cholesterol molecules between specific cells and tissues that is necessary with changes in dietary fatty acid supply. The authors conclude that hence, circulating levels of LDL cholesterol may change for non-pathological reasons: a saturated fat-induced elevation in LDL cholesterol in healthy individuals could represent a normal rather than a pathologic response.
To summarize this mechanism: In healthy people, the increase in LDL observed after adopting a diet high in saturated fat is a normal, adaptive mechanism to preserve optimal cellular function—not a pathological response, as is often assumed. Thus, the interpretation of cholesterol markers should be assessed based on the individual’s diet.
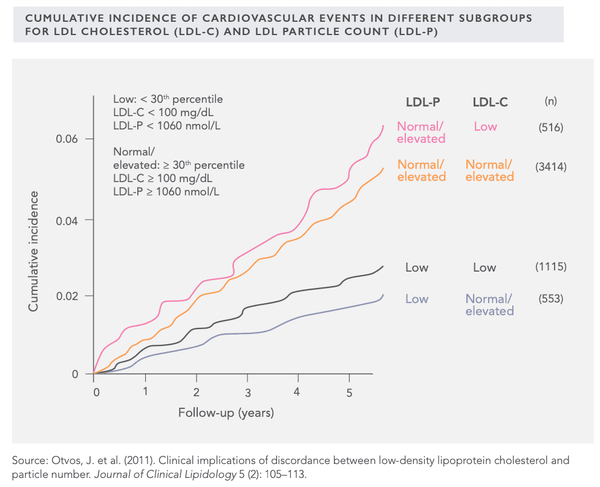
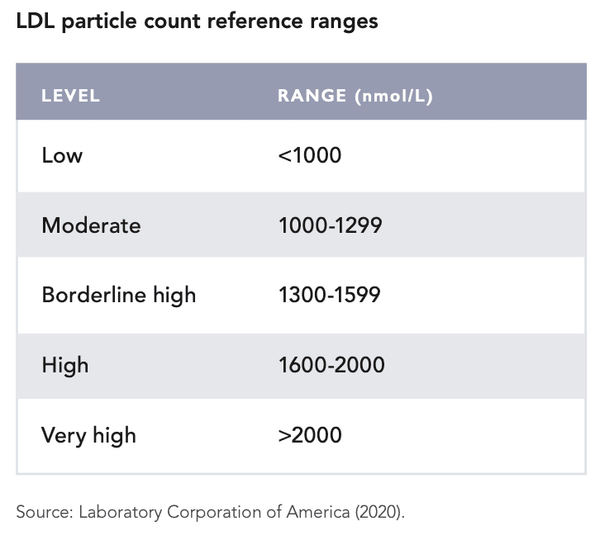
NB! Rather than LDL cholesterol, a better indicator of cardiovascular disease risk is the LDL particle count (see above). Significant discrepancy may occur between LDL cholesterol and LDL particle counts (i.e., LDL cholesterol may be high while the LDL particle count is proportionally much lower). On the other hand, the opposite may also apply (lower LDL cholesterol, higher LDL particle count). From the image on the previous page, it can be seen that low LDL particle counts are always associated with lower cardiovascular mortality. Mortality is lowest when LDL-P is low (less than 1,060 mmol/L) but LDL cholesterol is higher (more than 2.6 mmol/L).
A low-carbohydrate diet has been commonly found to be a significantly more effective method for weight-loss and lowering the risk of cardiovascular disease compared to a low-fat diet, despite the slight increase in LDL cholesterol levels caused by it. A low-carb diet usually results in a decreased LDL particle count while increasing HDL cholesterol levels and the size of LDL cholesterol – a change with health benefits (cf. small LDL cholesterol size). The amount of harmful very-low-density lipoprotein (VLDL) cholesterol has also been reduced by following a low carb/ ketogenic diet.
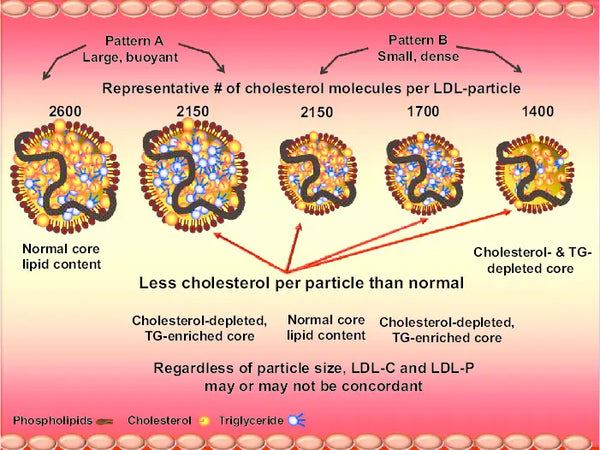
Image: Low-density lipoprotein (LDL) composition: depending on LDL particle size and composition, LDL cholesterol and LDL particle number may or may not be concordant. Depending on the cholesterol/triglyceride (TG) composition, both large and/or small particles may be cholesterol depleted, which will therefore require more LDL particles to traffic a given amount of cholesterol.
Source: Dayspring, T. & Dall, T. & Abuhajir, M. (2010). Moving beyond LDL-C: incorporating lipoprotein particle numbers and geometric parameters to improve clinical outcomes. Research Reports in Clinical Cardiology 1: 1-10.
However, it should be noted that the low-carb/ketogenic (high-fat) diet is not suitable for some individuals, most likely due to genetic reasons (such as the ApoE 4/4 gene variant, familial hypercholesterolemia, or ApoA2 CC gene variant). In these cases the anti-inflammatory diet is also beneficial, although in terms of carbohydrate intake it should resemble the Mediterranean diet where the role of cold-pressed olive oil is highly significant as a fat source (at the same time reducing the intake of saturated fat) while not dramatically restricting the consumption of carbohydrates.
In 2004, the Nordic Reference Interval Project (NORIP) determined the reference range for LDL cholesterol for healthy adults:
The reference range for adults according to the NORIP study:
- Aged 18–29: 1.2–4.3 mmol/L or 46.4–166.3 mg/dL
- Aged 30–49: 1.4–4.7 mmol/L or 54.1–181.8 mg/dL
- Aged 50+: 2.0–5.3 mmol/L or 77.3–205 mg/dL
The ratio of total cholesterol to HDL cholesterol is a good indicator of the risk of cardiovascular mortality. The TC/ HDL-C ratio reflects how long LDL particles remain in the blood. The longer they circulate in the blood, the more prone they are to oxidative stress caused by free radicals, and thus oxidation (so-called oxidized LDL-C).75 Oxidized LDL cholesterol is particularly harmful to blood vessels.
Important notes for the optimization of cholesterol levels with dietary macronutrients:
- In relation to saturated fat, changes in cholesterol levels are heterogeneous and individual.
- For saturated fat, the cholesterol-increasing effects are highly dependent on the length of the fatty acid carbon chain – the longer the chain, the smaller the impact on cholesterol.
- Stearic acid (saturated fat, C18) always lowers the LDL cholesterol slightly and does not increase the risk of artery thrombosis – stearic acid can be found in foods such as dark chocolate (43%) and to some extent in butter, meat, and eggs.
- The intake of saturated fat COMBINED with a carbohydrate-rich diet causes cholesterol values to deteriorate and forms a predisposing factor for metabolic syndrome.
- Of saturated fats, palmitic acid (C16) was previously considered to be harmful to the cardiovascular system due to its tendency to slightly elevate LDL cholesterol values. However, latest study reviews indicate that this conclusion is incorrect – replacing the intake of saturated fat with carbohydrates has been found to increase the risk of cardiovascular disease. Palmitic acid can be found in foods such as butter (29%), dark chocolate (34%), salmon (29%), and ground beef (26%).
- Myristic acid (C14) raises cholesterol levels slightly – myristic acid is plentiful in coconut oil (18% of total fat content) and can also be found in butter (11%)
- The cholesterol present in food does not significantly impact the cholesterol levels in the blood.
- Restricting saturated fat and proportionally adding monounsaturated fatty acids commonly lowers cholesterol levels (total cholesterol, LDL, and HDL).
- Replacing saturated fat with carbohydrates increases triglyceride levels (an unfavorable change).
- Carbohydrate-rich diets decrease the size of LDL particles and increase their density (an unfavorable change).
Important notes for the optimization of cholesterol levels with exercise:
-
Physical activity generally lowers the risk of cardiovascular disease, partially through improved cholesterol levels in the blood.
-
Brisk walking for more than 150 minutes per week reduces the risk of cardiovascular diseases and terminal events by 35%.
- Physical activity increases HDL cholesterol levels and decreases triglyceride levels.
- The impact of low-intensity aerobic exercise on the cholesterol levels in the blood varies on an individual basis – the most common change is a slight increase in HDL cholesterol.
- More intense aerobic exercise improves LDL cholesterol and triglyceride levels.
- The frequency of aerobic exercise appears to trump intensity when optimizing the cholesterol values in the blood.
- Strength training improves blood cholesterol levels (medium and high intensity), reduces triglyceride levels, reduces LDL cholesterol levels, and reduces total cholesterol/HDL cholesterol ratio.
- Cross-training reduces LDL cholesterol levels.





