Is the gut really our second brain? What is the gut-brain axis? How does improving your gut health improve the health and function of your brain? Everything about probiotics, prebiotics, gut supplements, diet and much more in this article. Read on!
Introduction
The gut-brain axis refers to the connection between the nervous system of intestines (the enteric nervous system) and the central nervous system (the brain and the spinal cord). There is indeed a direct neurological and biochemical link between gut health and the function of the brain. Sometimes the gut is even called “the second brain.’’ The intestinal microbiota (bacterial strain) affects the function of the immune system, the function of the nervous system, behavior, stress tolerance, mood and mental health. Recently, there has been a growing understanding of how important intestinal health is for the wellbeing of the brain.
In one study, researchers compared the effects of microbiota in cognitive functioning. Researchers first transplanted two different kinds of stool samples from humans into the intestines of mice. One group of mice got stool from humans with schizophrenia and the other group got stool from a mentally stable and generally healthy group of people. As a result, the mice who got the transplant from schizophrenic patients developed symptoms of hyperactivity and struggled with cognitive tasks. The other group, who got stool from healthy humans, had normal cognitive functioning and mood.
Importantly, researchers noticed that after the transplant, the mice groups had different levels of important brain hormones such as glutamate, glutamine and GABA – especially in the hippocampus. This led the researchers to conclude that the differences in the (transplanted) gut microbiota modulated the levels of the brain hormones in these mice, which in turn changed their behavior.
Gut health is also linked to brain growth and neuroplasticity. For example, chronic gut inflammation is linked to imbalances in brain hormones and lower levels of brain growth factor, whereas a healthy gut contributes to a better mood, stable energy levels and better cognitive performance.
Researchers at the University of Alabama made a potentially groundbreaking discovery about the brain in 2018. According to their preliminary study, they found out there are living bacteria in the brain. Most of the bacteria were from three phyla common to the gut: Firmicutes, Proteobacteria and Bacteroidetes. This finding is yet to be scientifically repeated and verified by further studies.
Gut microbiota means the collection of microbes that live inside the gut (in the intestines). These include bacteria, fungi and viruses, some of which are linked to better health and others that are linked to disease (so-called “good” and “bad” microbes, respectively). There are about 10 trillion microbes in the gut. The composition of the microbiota is unique and individual – thus, it’s like a fingerprint in the gut.
The microbial community, including the beneficial bacteria, support health by living in a mutual synergy with the host organism. Microbiota helps in strengthening the surface of the intestines, metabolizing energy from foods, protecting the body from bad bacteria and processing bile acids. Importantly, the gut microbiota has strong links to brain functioning. A balanced microbiota is linked to improved cognition and better overall health. For example, 95 % of the neurotransmitter serotonin (important for memory, mood and co-operative behavior) is produced in the gut. For that reason, gut problems such as celiac disease, IBS, leaky gut and upset stomach can lead to brain fog, anxiety, lowered mood, slowed thinking and decreased stress tolerance.
How healthy gut microbiota affects mental functioning:
- Produces most neurotransmitters found in the human brain (serotonin, GABA, acetylcholine, dopamine and noradrenaline), some of which travel to the brain
- Reduces hypervigilance and stress by balancing HPA- activation
- Involved in synaptic maturation and neuroplastic changes
- Affects the maturation of brain areas linked to memory and mood (hippocampal serotonergic system)
-
Offers nutrients for brain cells and supporting brain cells (glial cells), which are important for fast thinking and brain detoxification
HOW THE GUT AND THE BRAIN ARE CONNECTED
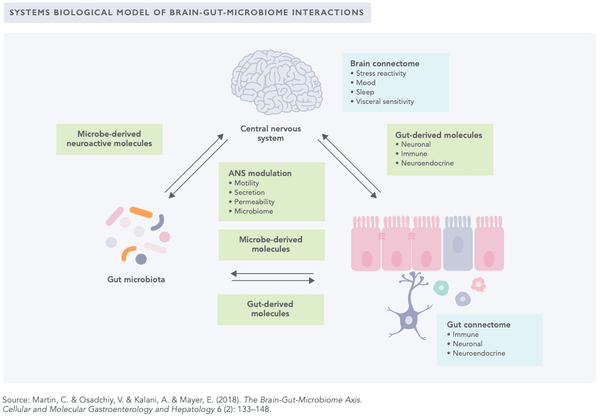
To better understand how your brain health is affected by gut health, it is important to understand the nature of the communication between the brain and intestines. Recent studies strongly suggest that there is a bi-directional brain-gut-microbiota (BGM) interaction. A good example of brain-to-gut connection is a strong emotional reaction, such as an experience of fear or love. During such a reaction, the changes in the brain’s emotional processing alters the function of the nervous system (including the vagus nerve) and modulates the activity of the intestines, causing the sensation of “butterflies in the stomach.”
Another good example of gut-to-brain connection is after eating, when the intestines send the brain information about the food eaten. The first signs of impaired brain function may also be detectable in the digestion: the impaired secretion of pancreatic enzymes, weak gallbladder activity and the general impairment of intestinal balance and function.
Microbiome and microbiota are sometimes used interchangeably, but these two terms have clear differences. The microbiome refers to the collection of genomes from all the microorganisms in the environment. For example, the human microbiome refers to a collection of microorganisms all around the body (including skin microbiome, eye microbiome, gut microbiome and so on). Microbiota usually refers to specific microorganisms that are found within a specific environment. In this case, microbiota (i.e., gut microbiota) refers to all micro-organisms, such as bacteria, viruses and fungi found in the gut.
Gut and the brain are linked in several ways:
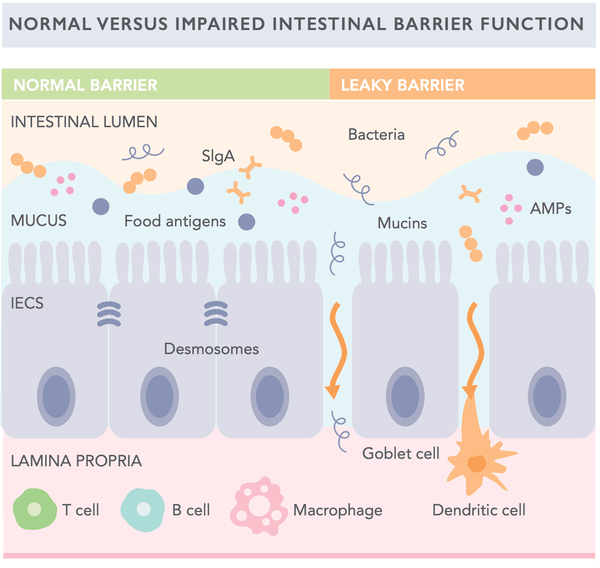
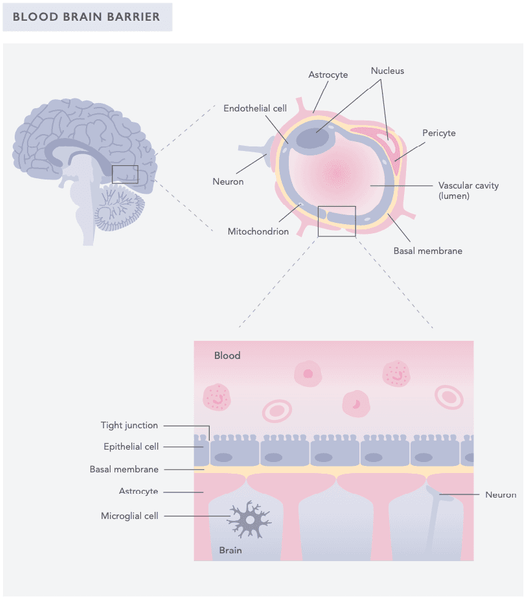
There are two natural barriers within the brain-gut- microbiota axis: the intestinal barrier (IB) and the blood-brain barrier (BBB). The intestinal barrier (IB) protects the intestines from harmful agents such as toxins. It has two layers: a basal monolayer of epithelial cells interconnected by tight junctions and a mucus layer whose thickness and composition changes over time and contains secretory IgA and antimicrobial peptides.
The blood-brain barrier (BBB) is a protective layer found in the blood vessels around the brain and the central nervous system. It prevents unrecognized molecules from the bloodstream (including toxins and even some medications) to enter the brain. It’s made of three types of cells: endothelial cells, astrocyte end-feet and pericytes.
The permeability of both layers can be modulated by gut health, gut microbes, stress and inflammation. They also affect the information flow between the gut and the brain. Thus, intestinal health plays a major role in brain health, emotion regulation and overall wellbeing and balance of both mind and body.
Five most important links between the brain and the gut:
1. The vagus nerve. Vagus nerve connects the brain to several internal organs (for example gut, lungs, heart, liver and kidneys). Gut modulates the functions of the brain and central nervous system mainly via hormonal and neuroimmune mechanisms, which often involves the vagus nerve. Molecules in the gut also play a part. These include short-chain fatty acids (SCFAs), secondary bile acids and tryptophan metabolites.
2. Sympathetic and parasympathetic nervous system. Both branches of the autonomic nervous system (ANS) contribute to the signaling between the gut and the brain. They regulate gut functions linked to bowel movement, gastric acids, gut fluids, gut cell structure, gut permeability and gut immune response. These important changes in gut physiology affect the gut microbiome and its composition.
3. Neurotransmitters and hormones that are produced in the gut. Hormones that are linked to motivation and mood, such as serotonin and dopamine are also produced in the gut and modulate gut activity. Their precursors (i.e., tryptophan and tyrosine, respectively) can also travel to the brain via the blood, cross the blood-brain barrier (BBB) and are used in hormone production in the brain. The specific mechanism of gut hormones in neuromodulation is still unclear, but it is believed that the ability to produce hormones such as serotonin and dopamine in the gut affects mood and brain function.
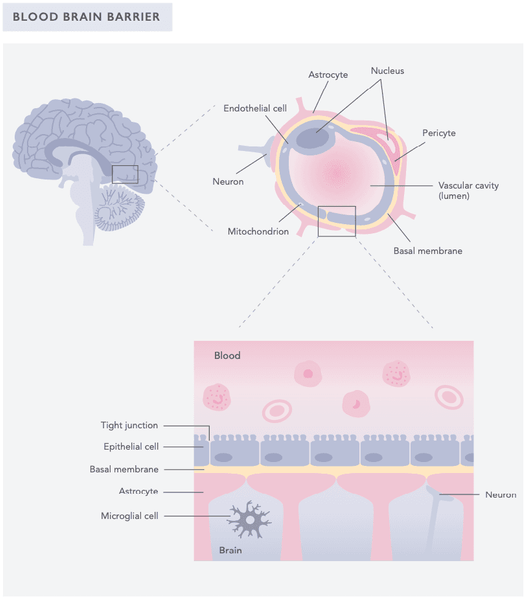
4. Chemicals and molecules that alter the function of the blood-brain barrier (BBB). BBB regulates traffic between the blood and the cerebrospinal fluid of the brain and the central nervous system. Gut microbiota and several microbially-driven molecules can up-regulate the expression of tight junction proteins, therefore decreasing BBB permeability.
5. Blood-brain barrier. BBB protects the brain from harmful pathogens and improves overall immunity of the brain.
1. VAGUS NERVE
The vagus nerve is a long nerve (10th cranial nerve) that connects the brain to several internal organs such as the gut. It consists of two separate branches on the right and left side of the spinal cord. The vagus nerve regulates virtually all of the functions of the internal organs such as heart rate, respiratory rate, bowel movement and sweating, including the contraction of the muscles involved in talking and eating. It also regulates the stress response and affects emotions via the hypothalamic-pituitary-adrenal (HPA) axis.
The vagus nerve transmits a huge amount of information to all directions in the body. It informs the brain about the condition of the intestines via the efferent nerve branches, but it also delivers information from several organs to the brain via afferent nerves. These include information from facial contact and pain, outer ear temperature and cerebral tension via trigeminal nerve nucleus (Lat. nucleus mesencephalic trigeminalis) and messages from the taste buds (as well as internal organs) via the nucleus solitarius. The afferent nerve fibers comprise about 80 % of the vagus nerve.
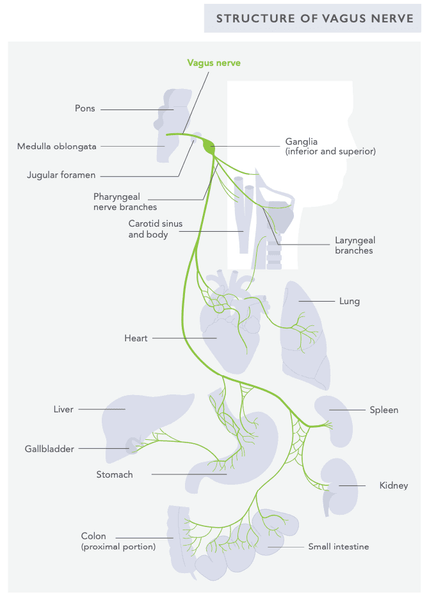
The vagus nerve powers and activates the parasympathetic nervous system (“rest & digest”), thus increasing vagal activity, often called vagal tone, which is linked to a calm and content mood. When the vagus nerve activity s chronically low, the person can experience insomnia, anxiety and stress. Low vagus activity is also linked to gut problems such as IBS and IBD.
In the intestines, vagus nerve activation improves digestion, bowel movements and digestive fluid flow. It also slows down heart rate and increases oxygen flow to the heart. Gut microbiota can stimulate the vagus nerve, increase mood and improve stress resilience. Poor gut microbiota increases stress hormone levels, whereas normalizing gut microbiota (for example, with probiotic treatment) has been shown to bring stress hormone levels back to normal.
Increasing vagus nerve activity also increases brain plasticity and brain cell growth and renewal in the hippocampus and cortex.
2. GUT MICROBIOTA & THE AUTONOMIC
NERVOUS SYSTEM
The autonomic nervous system (ANS) and its main parts, the sympathetic and parasympathetic branches, regulate the body’s immediate stress responses. ANS regulates gut functions, including bowel movement, secretion of gastric fluids, gut cell structure and mucus, antimicrobial peptides, intestinal permeability and gut mucosal immune response. Exposure to psychological, physical and environmental stressors cause gut dysbiosis (disruption in the balance of the microbiota). For example, a social stressor can affect microbial populations that are closely associated with the colonic mucosa (such as Lactobacilli species).
A growing number of studies also link maternal prenatal stress to the infant’s physical development and health and psychological functioning and behavior. For example, stress during pregnancy predisposes the baby to low birth weight and respiratory diseases. Altered composition of the microbiota and changes in colonization pattern also predisposes the developing infant to gastrointestinal symptoms and allergic reactions. Children of prenatally stressed mothers often show more impulsivity, anxiety problems, ADHD symptoms and worse cognitive and psychomotor development.
Stress can also cause the so-called leaky gut syndrome (see earlier) by two mechanisms: direct modulation of epithelial permeability (i.e., gut leakiness) and alterations in the intestinal mucosal layer (i.e., intestinal barrier). Gut leakiness allows bacteria and inflammation-causing molecules (e.g., lipopolysaccharides) to travel freely between the bloodstream and the gut, leading to increased inflammation in the gut. The intestinal mucosa thickness is modulated by ANS. Psychological stress can weaken the composition and size of the layer because of increased stress hormones such as noradrenaline and adrenaline. This means less protection on the surface of the gut.
3. HORMONES
Several gut hormones (or hormones produced in the gut) can travel to the brain, cross the protecting blood-brain barrier and alter brain function, mood, behavior and energy levels. For example, leptin, ghrelin, insulin, amylin and pancreatic polypeptides are part of such agents. Interestingly, hormones can have a different effect on the brain than in the body. Some gut hormones can also alter the functions of the blood-brain barrier. For example, insulin injection in the periphery (outside of the central nervous system) increases blood insulin levels and reduces glucose levels in the blood and stimulates feeding in animals. However, when insulin is administered in the brain, it will reduce blood insulin levels, increase blood glucose levels and inhibit feeding.
Insulin can also increase the transportation of tryptophan to the brain. Tryptophan is a precursor of the brain hormone or neurotransmitter serotonin, which is needed for content mood, cooperative behavior and proper sleep. Because humans are unable to produce tryptophan, dietary intake of proteins that contain it is the main source of tryptophan for humans. Gut microbiota contribute to the availability of tryptophan, which is needed to produce neurotransmitters and hormone serotonin.
Serotonin has important functions in the central nervous system regulating mood, memory and sleep. Serotonin (5-HT) is produced by the enterochromaffin cells (ECCs) of the gastrointestinal tract; approximately 95 % of the body’s serotonin is stored in ECCs and enteric neurons and only 5 % is stored in the central nervous system.
4. CHEMICALS AND MOLECULES PRODUCED
IN THE GUT
Several microbially-derived molecules, such as short- chain fatty acids (SCFAs) and secondary bile acids, transmit signals primarily through interaction with the surface of the gut including enteroendocrine cells
(EECs), enterochromaffin cells (ECCs) and the mucosal immune system. Some also cross the intestinal barrier, enter blood circulation and may cross the blood-brain barrier. Based on animal studies, the microbiota can also independently produce or contribute to the production of several neuroactive molecules including GABA, serotonin, norepinephrine and dopamine. However, it is yet unknown whether they reach relevant receptors or achieve sufficient levels to elicit a physiological response in the cells.
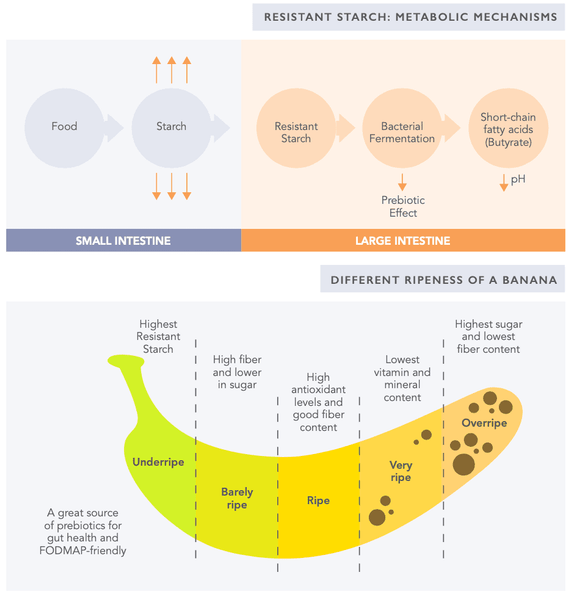
Short-chain fatty acids (SCFAs) help to deliver messages between the human organism and the microbiota via gut endocrine cells and the cells in the gastric glands (enterochromaffin cells). SCFA are generated by microbial fermentation of dietary fiber. They serve an important part in energy production while also stimulating intestinal blood flow, fluid and electrolyte uptake and repairing the gut lining. Dietary fiber (such as resistant starch and nonstarch polysaccharides) intake is a major regulatory factor of SCFA concentrations in the body (read more in the “Prebiotics” chapter below).
The influence of SCFAs has previously been identified to impact brain development and function including memory consolidation, the formation of new blood vessels, neurogenesis and BBB function. Recently it was discovered that gut flora may regulate the tightness and function of the BBB; mice that received gut flora-producing SCFAs (such as butyrate, acetate and propionate) had improvements in the function of the BBB. Propionate, in particular, has been shown to have protective effects upon the blood-brain barrier. For now, the exact mechanisms by which SCFAs produced by bacteria affect BBB maturity and function remains unknown.
5. BRAIN IMMUNITY AND PROTECTION
Immune system activation is strongly linked to the function of the brain. Changes in the microbiota influence both innate (the one you’re born with) and adaptive immune (the one you develop) system activation in the intestines (see Biohacker’s Hanbdook’s special chapter on Immunity). The physiological inter-relationship between mother and the fetus during pregnancy (or maternal-fetal interface) and systemic circulation is also associated with various neuroinflammatory, neurodegenerative and psychiatric disorders. The central nervous system (CNS) and peripheral immune systems are thus important for communication across the gut-brain-microbiota axis.
When harmful microbes attack the body, immune cells recognize them as harmful molecules and activate the immune system. The recognition of the microbes (microbe-associated molecular patterns; MAMPs) is done by so-called pattern recognition receptors. One type of pattern recognition receptor is toll-like receptors (TLRs) that are found in the innate immune system cells and brain cells. Thus, certain microbes may directly trigger innate immune pathways to affect CNS function. Indeed, intestinal microbiota-derived TLRs can be found all over the body and in the blood during chronic inflammatory disorders.
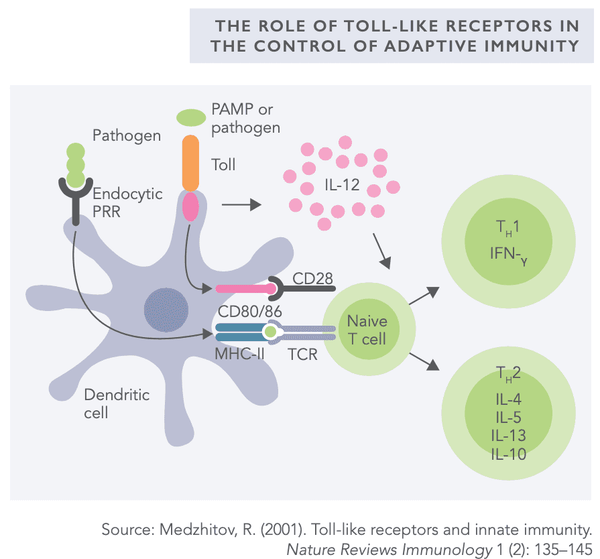
Intestinal bacteria have been shown to regulate fetal and adult neurogenesis in murine models. For example, bacterial cell wall components cross the maternal-fetal interface and activate TLR2 (toll-like receptor 2) that, due to excess neural proliferation (or increase), can cause impaired cognitive function during adulthood. Animal research suggests that maternal microbiota could influence offspring neurogenesis and subsequent behavioral changes. This means that the gut flora of the mother has a clear effect on the developing child’s future behavior.
Having a healthy gut microbiota is essential for the brain; it helps in clearing viruses and other pathogens, such as bacteria and fungi, from the nervous system and the brain. This was demonstrated in a study where researchers compared rats with a healthy “good” gut microbiota or with a bacteria-free microbiota (“bad” microbiota). First, they injected the mice with a virus that causes multiple sclerosis- type symptoms and then tracked their immune response. Only the mice with “good” microbiota could fight the virus and defend themselves from the symptoms of multiple sclerosis. Also, the mice with normal gut microbiota had more microglia in the brain – cells that support and protect the nerve cells. This led the researchers to the conclusion that a healthy gut microbiota helps in turning on an immune pathway, which can protect the central nervous system, including the brain.
SUPPORT YOUR GUT AND BRAIN WITH THESE FOODS
1. High-fiber foods
- Support healthy gut bacteria.
- Help digestive processes.
- Found, for example, in berries, cruciferous vegetables,
- nuts and seeds, mushrooms, fruit (such as avocados), legumes, roots and tubers.
Good supplemental sources of beneficial fiber:
- Psyllium
- Oat fiber
- Apple pectin
- Acacia fiber
-
You can also use resistant starch such as cooked and
then cooled white rice and potatoes
2. Probiotics and fermented foods
Fermentation is a process where bacteria or yeast break down carbohydrates in the foods that convert them into alcohol and acid. Fermentation has been used as a preservation method in many cultures for centuries. Lately, fermentation has been gaining more attention and its potential health benefits have been studied comprehensively. Probiotics in general, refer to living microbes that have positive effects on health. The benefits become apparent through the balancing of the microbiota in the digestive tract.
Benefits of probiotics include:
- Increases the levels of healthy bacteria, such as Lactobacilli and Bifidobacteria, and can help restore the natural balance of the gut flora
- Improves the condition of the gut surface (intestinal lining)
-
May help improve symptoms of mental health disorders
such as depression, anxiety, chronic stress and improve cognition and memory
Benefits of fermented foods include:
- Increases the bioavailability of the nutrients in food (meaning that the body can utilize important nutrients better)
- Contains plenty of healthy probiotics and improves digestive tract health
- Protects the brain from inflammation and harmful toxins
- Sauerkraut
- Fermented vegetables and their juices
- Yogurt
- Kefir
- Kombucha
- Kimchi
- Fermented teas
- Probiotics supplements are also available
N.B. When using probiotics in supplement form always beware of the indication you are using them so that you have a specific reason and focus for the usage. We also recommend that you measure the effects of supplemental probiotics in your gut microbiota. Probiotics may also possess side effects and can cause both local (gut) and systemic harm to the body.
3. Prebiotics
Prebiotics refer to indigestible fiber compounds that are essential for the growth of healthy bacteria in the intestine. These include oligo- and polysaccharides and fructans.
Potential gut and brain benefits of prebiotics include:
- Supports the growth of beneficial bacteria in the gut
-
May have positive effects on the absorption of trace
elements and on the immune system
Sources of prebiotics:
- Chicory root
- Artichokes
- Garlic
- Dandelion
- Greens
- Cocoa
- Asparagus
- Apples
- Raw bananas
-
Resistant starch in cold rice
and potatoes -
Grains or cereals also
have prebiotics but due to their potentially harmful anti-nutrients they are not recommended as brain foods.
4. Polyphenols
Increasing evidence suggests that polyphenols can protect the brain from oxidative stress and inflammation. Moreover, they can support cognitive functions. Polyphenol metabolites can directly act as neurotransmitters by crossing the blood-brain barrier or indirectly by modulating the blood supply in the brain.
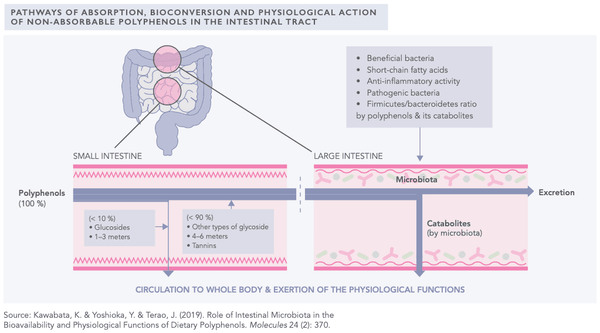
Potential gut and brain benefits of polyphenols include:
- Supports the growth of healthy gut bacteria.
- The total absorption of dietary polyphenols in the small intestine is approximately 10 %. The rest are transported into the large intestine where they are catabolized to phenolic acids by intestinal bacteria. Therefore, there is a significant functional interaction between polyphenols and intestinal bacteria.
- Lower inflammation in the gut.
- Activates short-chain fatty acid (SCFA) excretion in the gut.
- Improve intestinal immune system function.
-
Foods include for example dark/raw chocolate, citrus
fruits, extra virgin olive oil (EVOO), berries, almonds, green tea and herbs and spices.
Comment: High intake of various polyphenols is Dr. Sovijärvi's absolute favorite for improving gut and brain health!
///
Have you heard of the Gut-Brain -Axis previously? How do you support it? Tell us in the comments!
P.S. to optimize your brain and gut function, check out the Biohacker's Optimize Your Gut Online course
This article is an excerpt of the Biohacker's Brain Nutrition Guide. You can order the e-book here!





