Iron deficiency is the most common nutritional deficiency in the world. Globally, 25–30 % of the population is anemic. Half of these have anemia caused by iron deficiency. 1–2 % of American adults suffer from iron deficiency anemia. According to estimates, as many as 40 % of women have had iron deficiency anemia at some point during their lives. Iron deficiency is especially prevalent in developing countries, where malnutrition and poor nutrition are pervasive. However, also modern diet is to blame, which is often deficient in organ meats, shellfish, and dark green leafy vegetables.
Introduction
Iron deficiency can result in a weakened immune system, fatigue, and anemia. Iron is an essential mineral in many bodily processes, such as the production of hemoglobin, the oxygen-carrying molecule in the body. When iron levels are too low, the body may become deficient in hemoglobin, leading to anemia. This can cause symptoms like fatigue, breathlessness, and a weakened immune system, making it more difficult for the body to fight disease. Low iron levels can also affect cognitive development, as iron is necessary for neuronal growth and maturation.
Fortunately, there are many different ways to fix an iron deficiency. This article will explore the best sources of iron and other nutrients that improve iron absorption. We will also discuss foods to avoid when trying to increase your iron levels and some of the best plant-based and animal-sourced foods for fixing an iron deficiency.
The stages of iron deficiency:
- Iron stores running low (functional iron level in hemoglobin remains normal)
- Early functional iron deficiency before anemia becomes apparent
- Iron deficiency anemia (the hemoglobin level plummets below normal range; there is insufficient iron to enable normal red blood cell formation)
The first step in understanding how to fix iron deficiency is understanding the difference between heme and non-heme iron.
Heme vs. Non-Heme Iron
Heme iron is found in animal sources. It is easier for your body to absorb heme iron, making it a great way to increase overall iron levels.
Sources of heme iron include (per 100g):
- Organ meats (liver, kidney, heart, etc.): 6.5-12.2 mg
- Seafood (oysters, clams, mussels, etc.): 2.6-14.0 mg
- Red meat (beef, pork, lamb, etc.): 1.5-5.5 mg
- Poultry (chicken, turkey, duck, etc.): 0.7-4.4 mg
- Eggs: 1.4 mg
- Fish (salmon, tuna, mackerel, etc.): 0.3-3.3 mg
N.b. MFP Factor is a peptide present in meat, fish, and poultry. It enhances the absorption of non-heme iron present in the same meal. Studies consistently show an enhanced effect on vegetarian iron (non-heme) absorption by animal proteins. One study demonstrated that adding chicken, beef, or fish to a meal increased non-heme iron absorption by 2-3 times.
Non-heme iron, on the other hand, is found in plant sources, such as legumes, nuts, seeds, dark leafy greens, and certain grains.
Sources of non-heme iron include (per 100g):
- Dried basil (90 mg) and dried nettle (4.4 mg)
- Legumes (beans, lentils, peas, etc.): 3.2-9.7 mg
- Tofu and tempeh: 2.7-5.6 mg
- Dark green leafy vegetables (spinach, kale, collards, etc.): 0.8-6.4 mg
- Nuts and seeds (pumpkin, squash, sesame, etc.): 2-6.3 mg
- Dried fruits (apricots, raisins, prunes, etc.): 1.5-5.2 mg
- Whole grains (oats, quinoa, brown rice, etc.): 1.3-3.4 mg
Non-heme iron is more difficult to absorb by the body. Since plant sources are usually the only source of dietary iron in vegan and vegetarian diets, those individuals need to pay close attention to their iron levels. Also, phytates in cereals, nuts, and seeds prevent iron absorption.
About 25% of dietary heme iron gets absorbed, while 17% of dietary non-heme iron gets absorbed. Based on the studies, iron bioavailability is estimated to be 14–18% for a mixed diet and 5 to 12% for a vegetarian diet.
Sources of Heme Iron: Organ Meats and Organ Supplements
Organ meats can be beneficial for increasing iron intake and fixing iron deficiency. Organ meats are excellent sources of iron and contain high levels of vitamin A, copper, magnesium, and zinc, often co-deficient to iron.
Organ meats also include glandular that contain proteins, peptides, and other components similar to natural body tissues, which can help restore and promote the healthy function of your organs.
Top three organ foods for dietary sources of iron:
- The liver contains fat-soluble vitamins A, D, E, and K, along with proteins, carbohydrates, and minerals like zinc, copper, selenium, and iron.
- The kidney contains water-soluble vitamins such as niacin and vitamin C and essential minerals like phosphorus, potassium, and iron.
- The heart contains omega-3 fatty acids, iron, B vitamins such as folate, and electrolytes such as sodium and potassium.
Organ supplements can be an easy way to consume more organ foods, especially if you don't like the taste of organ meats. There are supplements for each organ, and a mix combines them all in one capsule.
Always ensure that your sources of organ meats and organ supplements are high quality, usually organic and grass-fed. Try out our recommended and trusted high-quality brand, Nordic Kings:
Grass Fed Organ Mix
|
Grass Fed Beef Liver
|
Other Sources of Heme Iron: Shellfish and Fish
Shellfish are a great source of dietary iron. These include shrimp, mussels, oysters, clams, and crabs. Additionally, seafood such as tuna, anchovies, salmon, and halibut are good iron sources.
Shellfish are also high in zinc, which helps your body absorb iron. Eating shellfish and fish with citrus fruits or vegetables like spinach or kale can also increase iron absorption into your system.
Eating shellfish or other seafood two or three times a week can help you meet your daily requirement for iron.
Sources of Non-Heme Iron
Plant-based foods that contain iron include:
- Legumes such as lentils, peas, kidney beans, and chickpeas
- Nuts and seeds such as brazil nuts, hazelnuts, almonds, and cashews
- Seeds such as pumpkin seeds and sunflower seeds
- Whole grains such as quinoa, bulgur wheat, and brown rice
- Dark leafy vegetables such as spinach, kale, swiss chard, and collard greens
- Dried fruit like raisins and apricots
- Seaweeds such as spirulina, kombu, wakame, nori and dulse
- Soybean-based such as tempeh and tofu
Herbs are a great way to add nutrition to your meals; many are high in iron. Herbs like oregano, parsley, basil, thyme, and sage are all excellent sources of dietary iron.
Mushrooms can also be an excellent source of dietary iron, providing up to 3 mg per cup. Common mushrooms such as white buttons, portobello, and shiitake contain iron. In addition to being high in iron, mushrooms are a great source of magnesium, calcium, potassium, zinc, B vitamins, and antioxidants.
Adding these vegetarian sources of iron to your diet can help, although note that the absorption will be better for foods including heme iron.
Iron-fortified foods like breakfast cereals and nut milks are not recommended due to the inclusion of problematic food additives, sugar, and other unnecessary ingredients. For the price, you also get less quality food which may damage your health. Therefore, start with whole foods.
Nutritional factors that inhibit iron absorption:
- Phytates (phytic acid) found in various foods (plentiful in pulses, whole grain cereals, nuts and seeds)
- Phenolic compounds in coffee, tea and herbal tea
- Soy protein (contains phytates)
- Calcium (inhibits the absorption of both heme iron and non-heme iron)
Iron Supplements to Complement Dietary Intake
It is best to get iron from natural food sources first. If you still have an issue with your iron levels, it may be a good idea to look into supplemental forms of iron. Iron sulfate is one of the most common forms of iron supplements. It may be the cheapest, but it is not the best for absorption (although fairly good) and can cause gastrointestinal side effects.
Better supplemental forms of iron include:
- Iron gluconate is a high-quality form of iron; this can provide high absorption rates, just like iron sulfate, but often causes fewer gastrointestinal side effects. The gluconic acid molecule helps regulate blood sugar levels, acts as an antioxidant, and may help protect against oxidative stress. Gluconate may also help to reduce inflammation and aid in wound healing.
- Iron bisglycinate is an even better form of iron that is highly bioavailable and easily digested. It is much less likely to cause gastrointestinal side effects. It has a glycin molecule in it that is related to tissue synthesis, neurotransmitter formation, and reduction in inflammation. Great versions include patented Albion Ferrochel and Iron Bisglycinate Chelate.
- Iron fumarate is exceptionally absorbable. It has a fumaric acid molecule, a precursor to the neurotransmitter glutamate, and can aid in regenerating cells and tissues. Fumaric acid has been linked to improved immune function and cardiovascular health and may even help reduce cancer risk. Additionally, it may play a role in controlling blood sugar levels, increasing energy production, and promoting weight loss. Combining these two elements allows for increased absorption in the body and fewer side effects than other forms of iron supplementation.
N.b. Interestingly, a 2020 study on iron-deficient anemic women shows that iron absorption from supplements is greater with alternate-day dosing than with consecutive-day dosing.
Our recommended iron supplements:
Ecosh Iron Bis-Glycinate
|
Ecosh Ferroschel® Iron Complex (with nettle)
|
Nutrients for Iron Absorption and Regulation of Iron Balance in the Body
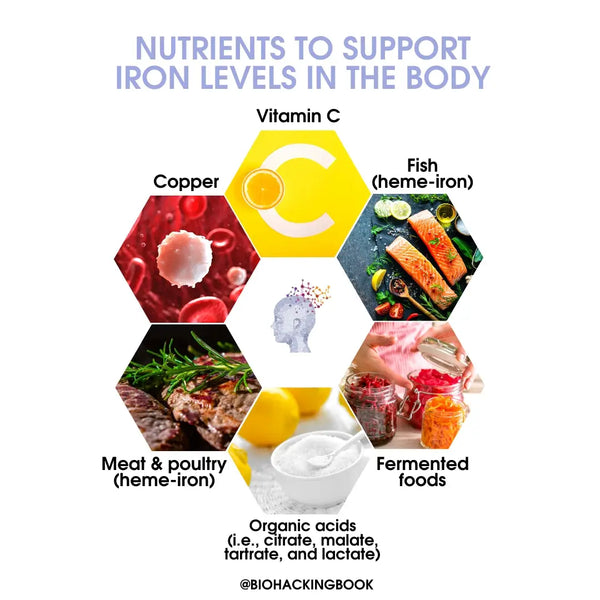
Certain nutrients can help the body absorb and use iron better and faster. These include:
- Vitamin C has been shown to enhance iron absorption significantly, and some experts suggest that taking it alongside iron can increase absorption by as much as threefold.
- Copper is another essential nutrient involved in iron absorption and transport in the body and is found in organ meats, shellfish, nuts, and dark chocolate.
- Vitamin B12 plays a vital role in the absorption of iron by helping to break down dietary proteins, supporting digestion, and red blood cell formation. It also helps to convert dietary iron into a form usable by the body. Vitamin B12 is found naturally in animal products such as meat, poultry, eggs, and fish.
- Vitamin A helps to increase the production of a protein called transferrin, which binds to dietary iron and helps transport it to the cells for absorption. Vitamin A also helps to create an acidic environment for iron absorption. Vitamin A is found naturally in animal products such as liver and eggs.
- Selenium helps to increase the activity of enzymes necessary for converting iron from dietary sources into forms usable by the body. Selenium is also essential for the healthy development of red blood cells, which help transport iron throughout the body. Selenium can be found naturally in certain foods such as Brazil nuts, tuna, and brown rice.
- Zinc helps the body convert dietary iron into a form that the body can use. Zinc also helps to regulate iron metabolism and is necessary for red blood cell production and healthy immune system function. Dietary sources of zinc include shellfish, red meat, beans, nuts, whole grains, and dairy products.
- Organic acids such as citrate, malate, tartrate and lactate; fermented foods in general
Iron absorption is worse if you are deficient in any of these nutrients, so make sure you get enough if you are trying to correct your iron deficiency.
Why Too Much Iron can be Unhealthy
Iron regulation in the body is very precise. In some cases, excessive iron may still occur as the body cannot excrete it. The most severe condition of excessive iron retention in the body is called "hereditary hemochromatosis." This disease is divided into four types based on the mutations. Most people suffering from hemochromatosis carry a homozygote mutation in the HFE gene (C282Y G>A.). Hereditary hemochromatosis may form a predisposing factor for many other illnesses due to the excessive iron retained in the body.
In addition to genetic risk, iron retention may be associated with metabolic syndrome or diabetes. In practice, this has been found in research situations where an individual has been diagnosed with elevated ferritin levels linked to elevated fasting blood sugar, insulin resistance, metabolic syndrome, and diabetes. In studies, this has been called "dysmetabolic iron overload syndrome" (DIOS). Such individuals have also been found to have elevated levels of hepcidin. This, in turn, may alter the genes that encode insulin production.
Excess iron (or hyperferritinemia) can be a problem because it can increase free radical production, which can cause oxidative damage to cells, proteins, and DNA. In addition, too much iron in the bloodstream can lead to increased levels of inflammation, which can further damage organs, tissues, and cells.
Excess iron can also interfere with the absorption of other minerals, making it difficult for the body to utilize essential nutrients properly.
Lastly, excess iron can accumulate in organs such as the heart, liver, and pancreas, leading to life-threatening conditions such as cirrhosis and heart failure (e.g. in hemochromatosis)
If you have excess iron, consider the following:
- Avoid the consumption of offal, game, and shellfish (these are rich in iron)
- Limit the consumption of lamb and beef to 2–3 times per week
- Limit the intake of vitamin C to 200 mg per day (vitamin C promotes iron absorption)
- Avoid the consumption of alcohol and sugar (these increase iron absorption in the intestine)
- Avoid taking multivitamins that contain iron
- Eat a wide variety of fruit and vegetables (these inhibit iron absorption and reduce the oxidative stress caused by iron)
- Drink coffee or tea with meals (tannins inhibit iron absorption)
- Grapefruit seed oil and green tea
- Some supplements, such as quercetin, resveratrol, Milk Thistle, EDTA, and DMSA, are also able to chelate heavy metals, including iron
- Blood donation
Excess iron may reduce your healthspan and even lifespan. If the issue continues, consult medical experts.
Genes Related to Iron Deficiency or Iron Overload
Genetic testing for iron deficiency or iron overload involves the evaluation of different markers to determine if an individual is predisposed to having this condition. Common markers used in genetic testing include HFE, SLC40A1, SLC11A2, and TMPRSS6.
HFE is a gene that codes for the protein hemochromatosis. This is a hereditary condition that causes an excess of iron in the body and can result in organ damage (see earlier).
SLC40A1 and SLC11A2 are two specialized genes responsible for controlling the movement of iron into and out of cells. Mutations in these genes can make it difficult for the body to process iron properly.
TMPRSS6 is a gene that helps regulate hepcidin, a hormone important in iron metabolism. When iron levels are low, hepcidin increases, prevents the absorption of more iron from the diet and blocks the release of stored iron from the body'sbody's reserves. Conversely, hepcidin decreases when iron levels are high, allowing more iron to enter circulation.
Genetic testing can help identify an individual'sindividual's risk for iron overload or deficiency, but the results should always be interpreted in conjunction with other findings, such as blood tests.
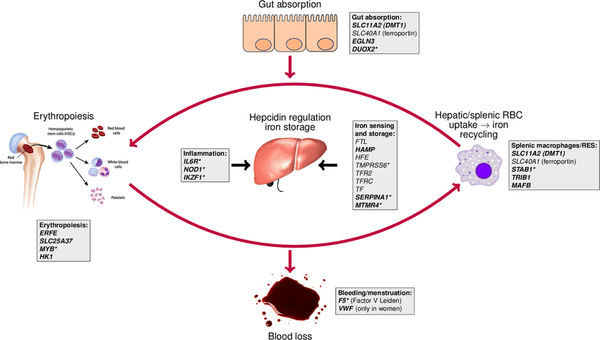
Image: Iron homeostasis loci (genes) in the context of systemic iron homeostasis.
Source: Bell, S. et al. (2021). A genome-wide meta-analysis yields 46 new loci associating with biomarkers of iron homeostasis. Communications biology 4 (1): 156–169.
Laboratory Testing for Iron Deficiency
Before supplementing on iron, it is highly recommended to ensure you have an iron deficiency or increased physiological need for iron, as excess iron can be damaging.
Laboratory testing for iron deficiency involves the evaluation of different biomarkers to determine if an individual is deficient in this essential mineral.
Common biomarkers used in testing:
- Ferritin is a central storage protein for iron and can be found in the liver, spleen, and bone marrow. Low levels of ferritin, called hypoferritinemia, occur when iron levels are low. However, note that high ferritin levels are associated with dysmetabolic iron overload syndrome (DIOS), most commonly associated with metabolic syndrome, diabetes, and insulin resistance. Therefore just measuring ferritin is not conclusive for measuring iron balance in the body.
- Serum iron is the level of free (unbound) iron in the blood, which can be measured to indicate how much iron is available for hemoglobin production.
- Serum transferrin saturation measures the amount of iron bound to the transport protein transferrin, with high levels indicating that more iron is being carried in the body.
- Transferrin levels, also known as the total iron-binding capacity, are used to assess how well the body can absorb iron from the diet.
Other iron studies for the evaluation of iron deficiency are:
- Soluble transferrin receptor (sTfR) and sTfR-ferritin index
- sTfR is elevated in iron deficiency because of the upregulation of transferrin receptors
- It can help differentiate between absolute (increased sTfR) and functional ID (normal sTfR)
- Zinc protoporphyrin/heme ratio
- Decreased iron supply for the formation of hemoglobin leads to increased utilization of zinc and an increase in the ZPP/H ratio
- Reticulocyte hemoglobin content
- Provides an estimate of iron availability for RBC production over a few days before the test
- A valuable indicator of early iron deficiency
The tests help to identify iron deficiencies and iron overload, as well as help identify specific medical conditions that may cause an iron deficiency, such as anemia, gastrointestinal bleeding, or malabsorption.
Conclusion
Iron deficiency can be a severe health concern, but fortunately, you can take many different steps to fix it. Understanding the difference between heme and non-heme iron and including both in your diet is essential for getting the recommended daily intake. Don't just take an iron supplement without considering co-dependencies and co-deficiencies. Our research and recent scientific findings suggest adding organ supplements, herbs, and shellfish into your diet is the best bet overall as they provide a full spectrum of necessary nutrients. Keeping these points in mind allows you to get your levels back up to where they should be in no time.
///