Vitamin D or Cholecalciferol (Vitamin D3)
Vitamin D is an exceptional substance as it is in fact a hormone precursor or a hormone-like substance. Vitamin D, indeed, affects the work of more than 2 000 genes and 37 different organs through the vitamin D receptor (VDR). There are several different forms of vitamin D that influence the body in various ways and in different places. The forms of vitamin D include vitamin D1, vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Of these, vitamin D3 is the main active hormone, which is produced by humans through solar UVB radiation in the skin, and later in the kidneys and liver.
THE SYNTHESIS OF VITAMIN D IN THE HUMAN BODY
Some seafood, fish oil, milk products, eggs and mushrooms contain vitamin D3 (mushrooms mostly contain vitamin D2). In most cases, the amount of vitamin D you get from food sources is not enough to meet your body's needs unless you are getting the sunlight all year round.
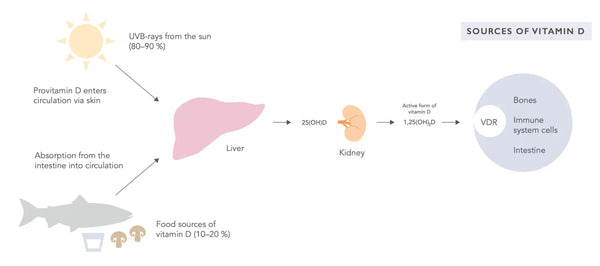
The precursors of vitamin D, which is physiologically active at the tissue level, that is, vitamins D2 and D3 are first hydrolyzed in the liver to form the inactive form of vitamin D storage - calcifediol (25(OH)D) (see the image above). Next, they are hydrolyzed in the kidneys to form calcitriol (1,25(OH)2D), which binds to the vitamin D receptors (VDR) in cells. Laboratory tests usually measure calcifediol. Generally, the reference values and the efficacy of vitamin D in the prevention of various diseases have been evaluated in terms of the calcifediol levels in the bloodstream.
Adequate intake of magnesium ensures the proper production of vitamin D in the skin and kidneys. Inadequate magnesium intake among the Finnish population contributes to vitamin D deficiency. Concomitant magnesium and vitamin D deficiencies negatively affect calcium metabolism, interfere with the proper functioning of the brain and immune system as well as predispose to the onset of autoimmune diseases and mental health issues.
It was discovered that vitamin D acts through the VDR receptors in the immune system, pancreas, heart, and blood vessels as well as in muscles and brain. In the past, the adequate intake of vitamin D was considered necessary only to prevent the onset of rickets and osteoporosis. However, recent research expertise demonstrates that the body uses vitamin D for different purposes.
The results of a study conducted by the University of Cambridge in 2014 have shown that human mortality was the lowest when vitamin D level in the blood (calcitriol) was at least 90 nmol/l. At that, a higher concentration of vitamin D in blood did not affect human mortality in any way.
Recent research suggests that vitamin D deficiency may pose a bigger threat to health than originally thought. The aim of the ongoing study FIND conducted by the University of Eastern Finland is to define the possible influence of vitamin D supplementation on the likelihood of developing cardiovascular diseases and cancers. In addition, this study aims at determining the effects of vitamin D supplementation on the course of other diseases such as Diabetes Type 2, depression, and bone health.
Test subjects are supposed to take either 0, 40 or 80 mcg of the supplement containing vitamin D. Apart from this supplement, the test subjects can consume up to 20 mcg of vitamin D supplement per day in accordance with current recommendations. The main result of the FIND study was that the use of significantly higher doses of vitamin D than recommended for five years did not affect the incidence or overall mortality of cardiovascular disease or cancer in elderly men and women.
In addition, the FIND study will further analyze and report on the effects of vitamin D supplementation on, among other things, the risk of type 2 diabetes, fractures and falls, mood, infections, and pain conditions.
- Osteoporosis
- Different cancers
- Diabetes (types 1 and 2)
- Cardiovascular diseases
- Different neurological disorders
- Psoriasis
- Different infections
- MS
- Asthma
- Blood pressure disorders
- Arthritis
- Sarcoidosis
- Sjogren’s syndrome
- Hashimoto disease
- SLE
- Scleroderma
VITAMIN D AND THE IMMUNE SYSTEM
Vitamin D plays a key role in the regulation of the immune system balance. For instance, vitamin D activates different T cells. In an immune response, a killer cell recognizes potentially harmful pathogens, captures, and presents them to a T-cell that produces vitamin D receptors (VDR). The receptor binds to vitamin D in the blood to activate T cells. As a result, helper T cells report the intruder and the killer T cells eventually try to get rid of the uninvited guest. Without vitamin D, T cells always stay dormant.
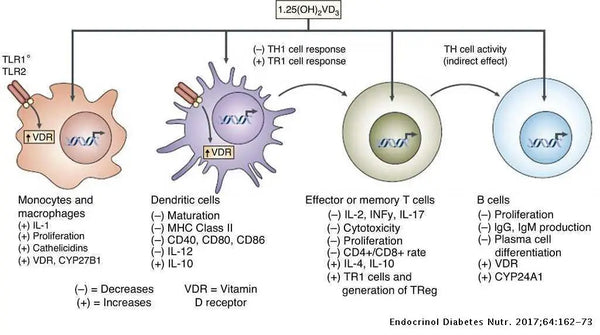
Image: The effects of vitamin D on the immune response.
Source: Rosas-Peralta, M. et al. (2017). Dysfunctional immunometabolic effects of vitamin D deficiency, increased cardiometabolic risk. Potential epidemiological alert in America? Endocrinología, Diabetes y Nutrición (English ed.) 64 (3): 162–173.
Vitamin D also directs the genes, which determine whether a T lymphocyte should become a killer, a helper, or a memory cell in the immune system. Vitamin D deficiency predisposes people to autoimmune diseases such as MS, diabetes, psoriasis, intestinal inflammation, and rheumatism. Moreover, people with the lowest blood vitamin D levels reported having more flu and common colds. Vitamin D deficiency also predisposes to silent inflammation, which underlies numerous chronic diseases. On the other hand, low blood vitamin D levels may also be due to chronic low-grade inflammation.
VITAMIN D: RECOMMENDED INTAKE AND REAL NEED
In Finland, for example, the official recommended daily intake of vitamin D for adults (18–74 years old) is 10 mcg. There is no need to take additional vitamin D supplements. The recommended daily intake of vitamin D for 2 weeks old babies and children under 2 years of age is 10 mcg and the additional requirement is 10 mcg a day. The recommended daily intake of vitamin D for children over the age of 2 is 7,5 mcg and the total daily intake is 10 mcg.
People over 75 years of age should take 20 mcg a day all year round. Pregnant and breastfeeding women should take 10 mcg of vitamin D supplement daily all year round. The average population-level daily intake of vitamin D supplements is 18 mcg.
A recent study by Finriski conducted by the Finnish Institute for Health and Welfare has determined the optimal vitamin D intake for Finnish people (Raulio etc. 2017). In 2012, the average serum 25(OH) vitamin D levels in those who did not take vitamin D supplements were almost 60 nmol/l. The average serum 25(OH) vitamin D levels of people who took vitamin D supplements were over 70 nmol/l, respectively. Adequate vitamin D intake over 80 nmol/l is required to ensure good bone health.
Still, the researchers concluded that: "The working-age adults do not need to take vitamin D supplements if they eat fish at least twice a week or regularly consume dairy products or fat spreads fortified with vitamin D."
Extensive research expertise shows that especially people with chronic diseases would need to keep the vitamin D intake at the level of 125–150 nmol/l. Professor of nutrition and epidemiology at the Harvard School of Public Health Edward Giovannucci states that serum vitamin D levels during the history of human development have been around 125 nmol/l most of the time. Nowadays, maintaining such a vitamin D level without using vitamin D supplements would be quite challenging.
The PANIC study (Physical Activity and Nutrition in Children) investigated the vitamin D intake of Finnish children, analyzing their blood values. The results of this study were published in 2016. Research has shown that the vitamin D intake of 6 to 8 years old children is very low. On average it was only 5.9 mcg (µg) per day. Only 40.8% of children took vitamin D supplements from a jar. Over 80% of children did not get the recommended dose of vitamin D in an amount of 10 mcg per day even though they were drinking milk fortified with vitamin D. Milk fortified with vitamin D provided almost half of children’s daily vitamin D intake. S-D-25 of every fifth child was under 50 nmol/l. Hence, they had a clear vitamin D deficiency (the internationally recommended vitamin D intake is 75–150 nmol/l).
According to the American Institute of Medicine (IOM), the recommended level of vitamin D (calcifediol) in the blood is 50 nmol/l. Still, IOM states that most of the population in Northern regions (97,5 %) maintain this level of vitamin D by ensuring daily intake of vitamin D in an amount of 15 mcg.
In 2014, the Finnish Medical Society Duodecim stated that:
"Canadian statisticians have proven the IOM calculation wrong. When the results of studies using IOM were analyzed again and the observed statistical error was amended, it was discovered that with the daily intake of vitamin D in an amount of 15 mcg the population’s level of calcifediol would certainly exceed the level of 27 nmol/l. The authors stated that the recommendation for too low daily vitamin D intake has serious implications for public health and negative therapeutic consequences and should be re-evaluated.”
According to a study published in 2017, the low recommendation for vitamin D intake in Finland could be based on erroneous statistical analysis. The National Nutrition Council of Finland is aware of this matter. However, recommended vitamin D intake has not yet been increased.20 Hence, it is very likely that the recommended vitamin D intake in Finland is not up to date. In the 1960s, the recommended daily amount of vitamin D was 100 mcg.
MEASURING VITAMIN D LEVELS IN LABORATORY
The level of vitamin D in the blood (S-D-25 or P-D-25/calcifediol) can be measured in a laboratory. The test can be done in any clinical laboratory. Calcifediol has seasonal fluctuations depending on the amount of sunlight unless a vitamin D supplement is taken. Individual variations can be large even granted the same vitamin D intake. This is due to genetic variations in the vitamin D binding proteins (DBP). Genetic studies show that DBP crucially affects individual serum vitamin D levels.
The half-life of S-D-25 is about three weeks whereas the half-life of the biologically active form of 1.25(OH)2D is only 4 to 6 hours. The concentration of calcifediol is better correlated with the clinical signs and findings of vitamin D deficiency and better reflects the body’s vitamin D storage and vitamin D intake than the concentration of vitamin 1,25(OH)2D, that is, calcitriol (S -D-1,25).
S-D-1,25 is generally used only in special cases when it is necessary to detect vitamin D 1α-hydroxylase deficiency or hereditary diseases affecting vitamin D metabolism. The level of calcitriol may rise during chronic infections. The latter might signify impaired functioning of vitamin D receptor.
Finnish reference values (Mineral Research Laboratory MILA Ltd.):
- Under 25 nmol/l: serious deficiency
- Under 50 nmol/l: the deficiency
- 50–75 nmol/l: generally considered sufficient
- 75–130 nmol/l: the target concentration
- Over 375 nmol/l: toxic concentration
According to the results of research conducted by the University of Birmingham and published in 2015, the recommended vitamin D values for the prevention of cardiovascular diseases are the following:
- Under 50 nmol/l: the deficiency
- 50–74 nmol/l: insufficient concentration
- 75–99 nmol/l: sufficient concentration
- 100–150 nmol/l: optimal concentration
- Over 375 nmol/l: toxic concentration
Adequate intake of vitamins A and K from nutrition protects against possible toxic effects of vitamin D overdose.
The Vitamin D Society’s recommended values are as follows:
- 0–100 nmol/l: the deficiency
- 100–200 nmol/l: sufficient concentration
- 200–250 nmol/l: high but normal concentration
- Over 375 nmol/l: toxic concentration
The following factors increase absorption and concentration of vitamin D:
- The best sources of vitamin D are the sun and UV radiation; it is recommended to stay in the midday sun for about 15–30 minutes daily depending on the skin type (NB: Many sunscreens prevent UV radiation from evoking efficient vitamin D production in the skin)
- Adequate vitamin A intake and its concentration in blood
- Adequate magnesium intake and its concentration in blood
- It changes the active form of vitamin D
- It helps with the transportation of vitamin D in the body
- Additional supplementation with the probiotic Lactobacillus Reuteri26
The following factors boost the functioning of the vitamin D receptor and its concentration:
- Physical exercise (excluding aerobic exercise)
- The neurotransmitter dopamine
- Bile and bile acids
- Omega-3 fatty acids (EPA and DHA)
- Curcumin
- Resveratrol
- Vitamin E
- Estrogen, testosterone, and phytoestrogens
The following factors block or weaken the functioning of vitamin D receptor (VDR) (meaning less active vitamin D and less advantageous cellular effects on the body):
- Caffeine
- Decreases VDR production
- Cortisol and glucocorticoids
- Antifungal medicine Ketoconazole
- Numerous different chronic infections:
- Helicobacter pylori, Pseudomonas aeruginosa, Borrelia, tuberculosis, Chlamydia (sexually transmitted disease), mononucleosis (Epstein-Barr virus), HIV, CMV, hepatitis C, Shigella and some systemic fungal infections
TOP FOODS THAT ARE HIGH IN VITAMIN D
(Source: The National Food Composition Database in Finland)
- Cod liver oil (1 tsp of 5–10 ml contains 10–20 mcg of vitamin D3)
- Eel and European river lamprey (25.6 mcg/100 g)
- Common whitefish (22.1 mcg/100 g)
- Canned herring (20.5 mcg/100 g)
- Funnel chanterelle (18.9 mcg/100 g)
- Baltic herring (17.9 mcg/100 g)
- European perch (16.8 mcg/100 g)
- Salmon (12.5 mcg/100 g)
- Egg yolk (7.2 mcg/100 g)
- Organic chicken egg (2.9 mcg/100 g)
- Different ready spreads fortified with vitamin D (about 10 mcg/100 g)
VITAMIN D SUPPLEMENTS
Choose from the available range of products the one that suits your needs. You can also ensure the proper intake of vitamin D by taking a slightly bigger dose corresponding to a large, pulsed dose of sunlight once a week. However, if vitamin D levels are chronically low, one should take vitamin D supplements daily until vitamin D levels are in the target range.
NB: It would be wise to measure the vitamin D level in the blood (calcifediol) before taking vitamin D supplements. It is also possible to overdose on vitamin D. This is largely due to individual genetic factors affecting the absorption and effectiveness of vitamin D. If you started to take the food supplement, please measure the vitamin D level in your blood again in about 3 months. This will allow you to assess the increase of vitamin D levels along with supplementation. In practice, many people certainly need higher doses of vitamin D than officially recommended. If the vitamin D level in the blood is low or not in the target range (generally it should be less than 70 nmol/l), one needs to take 50–100 mcg of vitamin D daily. The dose should be adjusted individually based on the blood test results. You can also get professional medical consultation in case of need.
If vitamin D level is too low (under 50 nmol/l), regular sun exposure is recommended (remember to consider your skin type so that you do not burn yourself!). Moreover, cod liver oil and suitable vitamin D supplement should be used in appropriate doses.
///





