Is it worth avoiding alcohol? Does eating liver improve liver function? Do supplements help liver function? Read more in this extensive article!
The liver is located in the top right corner of the abdominal cavity, immediately below the diaphragm, to the right of the stomach. Below it lies the gallbladder. Compared to other internal organs, the liver has a double blood supply via the portal vein and the hepatic arteries. This is indicative of the importance of the liver to the entire system. The liver is also a sizeable organ – it weighs on average 1.5 kg. More than 2,000 liters of blood flow through it every day.
The liver also contains the bile duct system, which collects the bile produced by the liver. Bile ducts generally refer to all ducts through which bile travels from the liver to the gallbladder and duodenum.
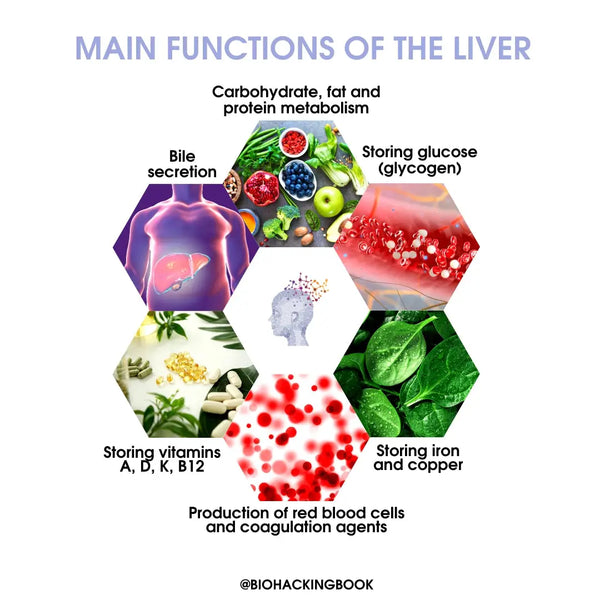
Main functions of the liver:
-
Carbohydrate metabolism:
- Produces glucose from amino acids, lactic acid, and glycerol
- Breaks down glycogen into glucose
- Forms glycogen from glucose
-
Fat metabolism:
- Oxidizes fatty acids into energy
- Produces large amounts of cholesterol, phospholipids and lipoproteins (such as LDL, HDL, VLDL)
- Protein metabolism:
- Breaks down amino acids
- Converts toxic ammonia into urea (urea cycle)
- Produces blood plasma proteins (including albumin)
- Produces amino acids and converts them into other compounds
- Bile secretion
- Production of red blood cells and coagulation agents
- Storing glucose (glycogen / 10% of the total weight of the liver), fat-soluble vitamins (A, D, K) and vitamin B12, iron, and copper
Cleaning and defense functions:
- Breaks down several hormones (including insulin)
- Breaks down and neutralizes toxins (detoxification)
- Removes (through urine) bilirubin released by red blood cells
Liver diseases and fatty-liver index
Liver disease-related mortality rates tripled between 1970 and 2010. And in the last decade especially non-alcoholic liver disease-caused mortality has increased dramatically both in the US and in Europe. Today's stressful work culture, alcohol use, problematic diet, and other environmental stressors have led to impaired liver function in many individuals. Abdominal obesity in particular contributes to the development of fatty liver disease. It has been estimated that a waist circumference exceeding 100 cm in men and 90 cm in women is a highly likely indicator of fatty liver disease. Recommended waist circumference figures are less than 94 cm for men and less than 80 cm for women. Approximately 80 % of individuals with BMI in excess of 30 have fatty liver disease. The most precise method of diagnosing fatty liver disease is by liver biopsy.
To determine the presence of non-alcoholic fatty liver disease (NAFLD), the so-called fatty liver index (FLI) can be utilized, factoring in the body mass index (BMI), waist circumference, blood triglyceride levels, and gamma-glutamyl transferase (GGT) levels.
The formula used to calculate FLI:
FLI = [e0.953 × ln (TG) + 0.139 × BMI + 0.718 × ln (GGT) + 0.053 × WC - 15.745/(1 + e0.953 × ln (TG) + 0.139 × BMI + 0.718 × ln (GGT) + 0.053 × WC - 15.745)] × 100
TG = Triglyceride in blood (mg/dL)
BMI = Body mass index
GGT = Gamma-glutamyl transferase in blood (U/I) WC = Waist circumference (cm)
Scientists have determined the following cut-off points for fatty liver disease: for men, 46.9 or greater; for women, 53.8 or greater. In practice, a value of less than 30 rules out fatty liver disease, whereas a value in excess of 60 is a certain indicator of the disease. The higher FLI value in women is thought to be due to the liver-protecting effect of estrogen. According to a comprehensive review, FLI is the most precise tool for the non-invasive assessment of fatty liver disease. However, simply measuring the waist circumference is nearly as accurate in determining non-alcoholic fatty liver disease.
Various medications also have a significant role in the development of liver damage. More than 900 drugs have been reported to cause liver damage. One half of all acute cases of liver failure are caused by various medications. Some medicinal herbal products may also be harmful to the liver.
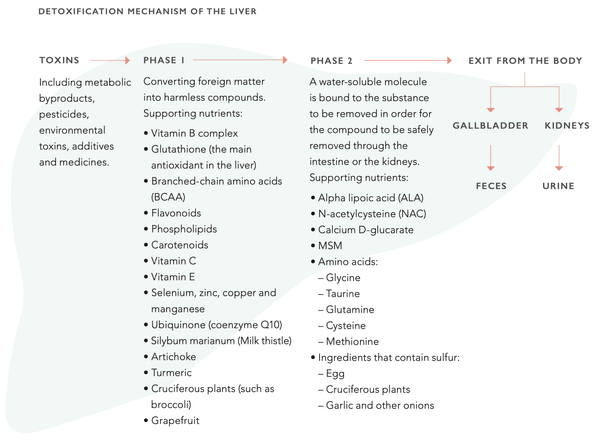
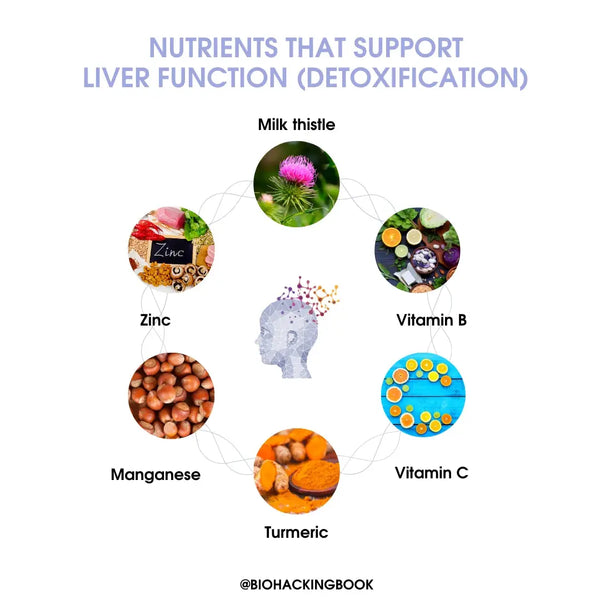
The liver has an astonishing ability to regenerate. Indeed, it is the only internal organ that can. Even when 75 % of the liver has been destroyed, it may return to a normal state. Liver function can be supported through nutrition. This involves supporting the cytochrome P450 enzyme system, which is central to the liver detoxification function. The system consists of two distinct phases (1 and 2). Both phases must run smoothly to maintain the optimal detoxification function of the liver.
Measuring liver function with blood biomarkers
Alanine aminotransferase (S-ALT)
Alanine aminotransferase (ALT) is an enzyme found most commonly in hepatocytes (the liver) and to a lesser extent the kidneys. Alanine aminotransferase also occurs in muscle cells, adipose tissue, the brain, and the prostate. The ALT enzyme catalyses the transfer of amino groups from L-alanine to alpha-ketoglutarate, producing L-glutamate and pyruvate. This chemical process is crucial for the mitochondrial citric acid cycle. Elevated ALT levels are usually indicative of liver damage caused by various illnesses – as liver cells are damaged, alanine aminotransferase is released into the circulation. The ALT levels in hepatocytes are 3,000 times higher than in the blood.
ALT levels may also be elevated due to heavy exercise (for up to a week afterward), alcohol use, hepatitis, celiac disease, certain medications (such as Paracetamol, statins, and opiate-based analgesics), and severe burns. Moderate increases in ALT levels also occur in connection with metabolic disorders such as hyperlipidemia, obesity, and type 2 diabetes. In many countries, the ALT levels are used to support the diagnosis of metabolic syndrome.
An increase in the ALT levels is directly proportional to the occurrence and severity of metabolic syndrome – the higher the ALT levels, the more likely and severe the metabolic syndrome.
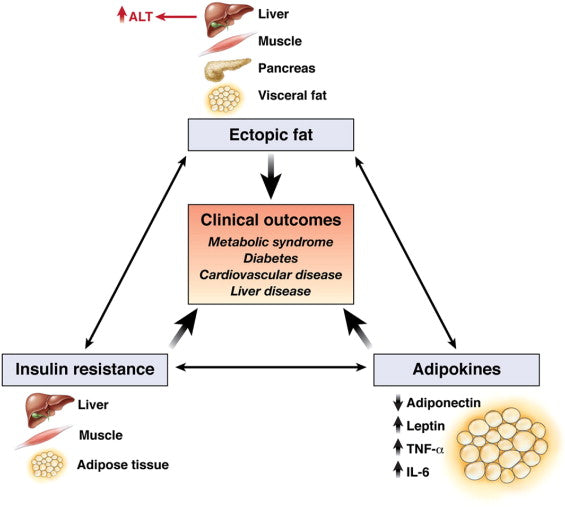
Image: Mechanisms that could explain why serum ALT level can also be a biomarker of cardiometabolic outcomes.
Source: Ioannou, G. N. (2008). Implications of elevated serum alanine aminotransferase levels: think outside the liver. Gastroenterology 135 (6): 1851-1854.
Extremely high ALT levels (10x the normal level) are usually caused by acute hepatitis. Elevated ALT levels are linked to increased mortality. Low ALT levels (below 10) are linked to higher mortality, particularly in the elderly. Low ALT levels may also occur in connection with impaired liver function.
Typical reference range (S-ALT):
- Women: below 35 U/I
- Men: below 50 U/I
Lifestyle factors decreasing ALT levels include:
- Weight loss, if the individual is overweight
- Hypocaloric diet (with a weight loss intent) in combination with cold-pressed olive oil will quickly reduce ALT levels in individuals with non-alcoholic fatty liver disease (NAFLD)
- Relatively low-carbohydrate (below 35 % / “Mediterranean”) diet
- Gluten-free diet (particularly for individuals with undiagnosed and/or untreated celiac disease)
-
A person with celiac disease whose liver function levels (incl. ALT) are elevated will often find that
these levels become normalized after a few months of consuming a gluten-free diet - Walking and basic aerobic exercise (particularly for individuals with non-alcoholic fatty liver disease or non-alcoholic steatohepatitis [NASH])
- Moderate-intensity strength training
- Coffee (and caffeine) may inhibit the rise of ALT levels to some extent (more than 2 cups per day vs. no coffee)
- Carotenoids from food reduce fatty liver disease and ALT levels
- For example, beta-cryptoxanthin and astaxanthin, also other carotenoids
- Vitamin E as a dietary supplement, particularly for individuals with advanced fatty liver disease and slightly elevated ALT levels, as well as individuals with NAFLD, NASH, or CHC (chronic hepatitis C)
- Resveratrol (500 mg/day) as a dietary supplement, particularly for individuals with advanced fatty liver disease
- Powdered (fermented) turmeric (3 g/day)
- N-acetylcysteine (NAC; 600 mg x2/day), particularly for individuals with non-alcoholic fatty liver disease
- Alpha-lipoic acid (400 mg/day) and ursodeoxycholic acid (300 mg/day), particularly for individuals with non-alcoholic fatty liver disease
- Artichoke leaf extract (2,700 mg/day) as a dietary supplement, particularly for individuals with steatohepatitis or NAFLD
- Probiotic therapy may reduce liver enzyme levels across the board and promote recovery from non-alcoholic fatty liver disease
- The mechanisms include reducing harmful bacteria, reducing small intestinal bacterial overgrowth (SIBO), regeneration of the intestinal lining, and immune system regulation
Aspartate Aminotransferase (S-AST)
Muscle cells, red blood cells, pancreas, kidneys, and the brain. There are two genetically distinct AST isoenzymes: mitochondrial AST (mAST) and cytosolic AST (cAST). Aspartate aminotransferase has an important role in amino acid and fatty acid metabolism. The AST enzyme catalyzes the transfer of amino groups from aspartate and alpha-ketoglutarate, producing oxaloacetate and glutamate. The chemical reaction also works in the opposite direction. Oxaloacetate has a crucial role in mitochondrial
energy production (citric acid cycle), urea cycle, and the breakdown and formation of glucose. The above-mentioned reaction requires bioactive vitamin B6 (pyridoxal-5-phosphate) as a cofactor.
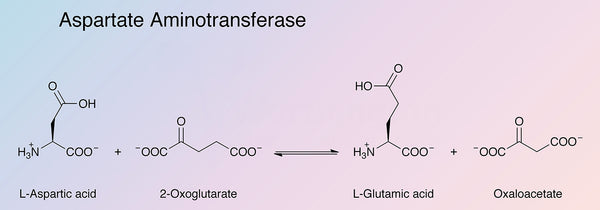
Image source: Worthington Biochemical.
AST levels increase in connection with cell damage. Due to this, it is used to assess damage to the liver or cardiac muscle (cardiac muscle damage is now predominantly assessed using various troponins, usually troponin-T). AST levels can also increase due to certain medications (Paracetamol and statins), chemotherapy, heavy exercise and rhabdomyolysis, acute pancreatitis or cardiac arrest.
Low AST levels sometimes occur in connection with vitamin B6 deficiency. AST may also be elevated in connection with cholestasis (bile duct obstruction) or various liver tumors and cancers. Acute viral hepatitis often causes AST levels 10 times higher compared to normal.
Elevated AST levels may also be a risk factor for future type 2 diabetes. This is particularly true if ALT levels are also elevated. Normal weight individuals with insulin resistance often also have elevated ALT levels but not AST. The AST/ALT ratio is under 1.
The AST/ALT ratio (De Ritis ratio) can be used to analyze an increase in AST levels – if the ratio is high, the increase is usually caused by tissues outside the liver. Usually the AST/ALT ratio is slightly above 1. The highest ratio (above 2) usually involves alcoholic hepatitis. Viral, drug induced, or
autoimmune hepatitis involves an AST/ALT ratio below 1.
Typical reference range (S-AST):
- Women: 15–35 U/l
- Men: 15–45 U/l
Nutritional factors decreasing AST levels include:
- Heavy coffee consumption (≥ 3 cups per day) is linked to lower AST levels, regardless of the caffeine content
- Silymarin extract (milk thistle; 200 mg x 3/day), particularly for individuals with type 2 diabetes
- Silymarin may repair liver damage and is generally well-tolerated
- Green tea extract (500 mg/day), particularly for individuals with non-alcoholic fatty liver disease
- A comprehensive meta-analysis on rat and human tests suggests that curcumin extract (dosage ≥ 1,000 mg/day) protects the liver from damage and reduces AST levels
-
Powdered turmeric (3 g/day)431
- Alpha-lipoic acid (400 mg/day) and ursodeoxycholic acid (300 mg/day), particularly for individuals with non-alcoholic fatty liver disease
- Alpha-lipoic acid (1,200 mg/day) reduces ALT and AST levels in obese individuals with NAFLD
Gamma-Glutamyl Transferase (GGT)
Gamma-glutamyl transferase (GGT) is an enzyme found mostly in the liver, but also in the kidneys, pancreas, and intestine. The main function of GGT is the breakdown and recycling of glutathione. GGT is also involved in the breakdown of many drugs and toxins, the formation of amino acids, and the conversion of inflammatory molecules into other molecules.
Elevated GGT levels occur predominantly in connection with liver diseases (hepatitis or cirrhosis), but also with heart failure, stroke, atherosclerosis, diabetes, anorexia, hyperthyroidism, cancer, or pancreatitis. The most common cause of high GGT values is alcohol abuse. Even small amounts of alcohol can increase GGT levels.
Elevated GGT levels also occur in approximately half of all cases of non-alcoholic fatty liver disease (NAFLD, see above). In such cases the levels are 2–3 times compared to normal. Many drugs can also increase GGT levels. These include anti-inflammatory drugs (NSAIDs), statins, antibiotics, antifungals, SSRIs, and H2 blockers. Environmental toxins can also increase GGT levels. Elevated GGT levels are linked to increased mortality. Low glutathione levels may also increase GGT levels, indicating that GGT levels are indicative of cellular level oxidative stress. Low GGT levels typically only occur in connection with familial intrahepatic cholestasis.
Elevated GGT levels are also an independent risk factor for type 2 diabetes (along with ALT) as well as an early predictive marker of atherosclerosis, heart failure, arteriosclerosis, gestational diabetes, and various liver diseases.
Alcohol-induced increase in GGT levels may be controlled with carotenoid-based antioxidants such as lycopene, alpha- and beta-carotene, and beta-cryptoxanthin. According to researchers, GGT may indeed be an early sign of oxidative stress in the body. The active form of ubiquinone, Ubiquinol
(150 mg/day), has been found to have a significant effect in reducing oxidative stress and GGT levels.
Typical reference range (S-GT):
- Women: below 40 U/I
- Men: below 60 U/I
Lifestyle factors reducing GGT levels include:
- Reducing alcohol use
- Carotenoids and Ubiquinol (see above)
- Avoiding heavy metals and insecticides as well as other pollutants
- Drinking coffee (particularly for men who use alcohol)
- Fish oil (a therapeutic dose, 4 g/day)
- Curcumin and turmeric
- The consumption of vegetables, berries, and fruits is linked to lower GGT levels
Conclusion
There is a lot you can do about your liver health lifestyle-wise. But at first, it is highly recommended to take at least these three liver biomarker tests and evaluate the condition of your liver. And even better would be taking these tests multiple times and regularly.
Learn more about optimizing your bloodwork HERE!
///
How do you support your liver? Tell us in the comments!
This article is a part of the unique Optimize Your Lab Results Online Course put together by Dr. Sovijärvi. Learn more about the course here and join in!





