Cet article explore l'importance cachée du thymus et examine des stratégies fondées sur des données probantes pour optimiser sa fonction afin d'améliorer l'immunité et le bien-être.
Introduction
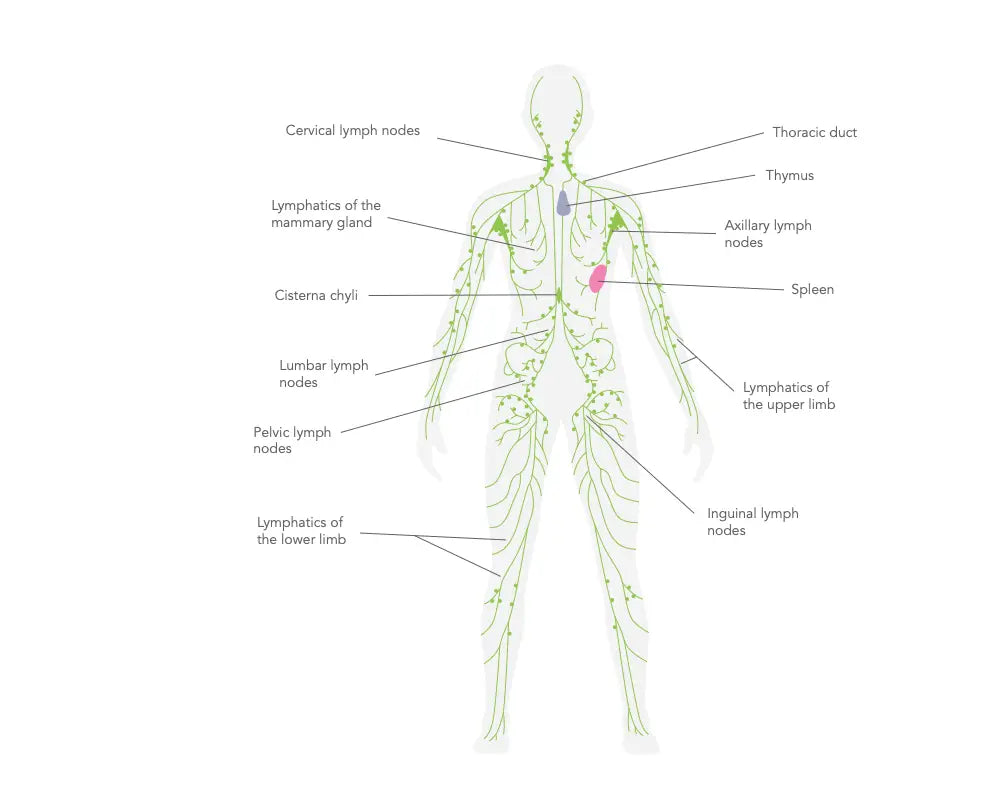
Le thymus est un organe lymphoïde primaire caractéristique du système immunitaire. Il se trouve dans le médiastin antéro-supérieur, en arrière du sternum et entre les poumons. Le thymus est une glande lobulaire composée de deux lobes distincts mais interconnectés. Chaque lobe est entouré et subdivisé en un grand nombre de lobules plus petits. Les lobules comprennent un cortex rempli de cellules T en développement et une médulla contenant des cellules T matures.(1)
Au cours de l'embryogenèse, le thymus se forme à partir des troisièmes poches pharyngiennes. Il augmente jusqu'à la puberté, puis entame une involution au cours de la vie. Cette involution se caractérise par le rétrécissement et le remplacement du tissu thymique par du tissu adipeux, ce qui fait que le thymus perd sa fonction avec l'âge.
Le rôle central du thymus est la synthèse et la maturation des lymphocytes T. Les thymocytes sont des cellules T immatures. Les thymocytes, cellules T immatures, naissent des cellules souches hématopoïétiques de la moelle osseuse et se déplacent vers le thymus. Là, ils sont soumis à une sélection très sévère. Le processus de sélection ne permet qu'à une infime partie des thymocytes de survivre, ce qui garantit que seuls les lymphocytes T présentant une restriction du CMH propre et une tolérance propre sont libérés dans la circulation.(2)
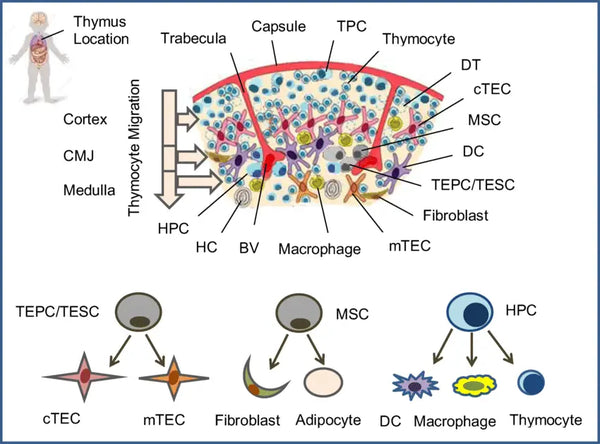
Image : Architecture des cellules du thymus humain.
Source : Shichkin, V. P. et Antica, M. (2020). Régénération du thymus et défis futurs. Revues et rapports sur les cellules souches, 16(2), 239-250.
Des recherches menées sur des modèles animaux ont montré qu'une variété d'hormones peptidiques et non peptidiques ont des rôles multiples dans le thymus, influençant la croissance, le développement, le mouvement et la mort cellulaire programmée (apoptose) des thymocytes au cours de leur maturation. Par exemple, des hormones comme l'hormone de croissance et la prolactine sont connues pour stimuler la croissance et le mouvement des thymocytes, tandis que les glucocorticoïdes ont tendance à déclencher l'apoptose de ces cellules.(3)
Les hormones du thymus et leurs effets sur l'organisme
Le thymus sécrète également plusieurs hormones, telles que la thymosine, la thymopoïétine et la thymuline. Ces hormones initient la différenciation et la maturation des cellules T. Il a été prouvé que la thymosine, en particulier, active la formation de cellules T dans d'autres organes lymphoïdes.
Thymosines
Un groupe d'hormones thymosines, la thymosine alpha-1 en particulier, est essentiel à la maturation des lymphocytes T.(4) La thymosine alpha-1 améliore les activités de certaines cellules immunitaires, telles que les cellules dendritiques et les cellules tueuses naturelles. Elle influence également la différenciation des cellules T et couvre un champ plus large que le seul thymus et ses activités impliquant les cellules T dans les tissus périphériques et d'autres organes lymphoïdes. Le potentiel de la thymosine en tant qu'agent thérapeutique a été largement étudié, en particulier pour le traitement des infections chroniques dans les états immunodéprimés et en tant qu'agent immunostimulant dans la thérapie du cancer.(5-6)
Thymopoïétine
La thymopoïétine influence la différenciation des cellules T et le processus de sélection des cellules T, permettant ainsi aux cellules T développées de répondre de manière appropriée aux pathogènes sans attaquer les tissus de l'organisme. La thymopoïétine contribue au développement de la tolérance immunitaire centrale, l'un des processus critiques de la prévention de l'auto-immunité. En outre, la thymopoïétine contrôle également la transmission neuromusculaire.(7-9)
Thymuline
La thymuline est une hormone nonapeptidique (un oligopeptide composé de neuf résidus d'acides aminés) sécrétée par les cellules épithéliales thymiques. Elle n'est active que lorsqu'elle est liée au zinc : la thymuline affecte le développement et l'activité des cellules T et d'autres types de cellules immunitaires. La fonction de la thymuline est essentielle dans la modulation de la réponse immunitaire, en particulier dans le maintien de l'équilibre entre les différents types de cellules immunitaires. En outre, les niveaux de thymuline diminuent au cours de la vieillesse, en corrélation avec les changements du système immunitaire liés à l'âge.(10-11)

Image : Une vision artistique des peptides thymiques.
Améliorer la fonction du thymus
L'amélioration de la fonction du thymus, en particulier chez les personnes âgées, est essentielle car le thymus est un organe crucial dans la régulation du système immunitaire. Aucune méthode spécifique n'est universellement acceptée pour améliorer la fonction thymique ; cependant, plusieurs approches peuvent être utiles.
Suppléments nutritionnels et régime alimentaire
Certains nutriments et suppléments ont été proposés pour améliorer la santé du thymus. Par exemple, le zinc et la vitamine D sont essentiels au système immunitaire et soutiennent la fonction thymique.(12) De nombreux récepteurs de la vitamine D (VDR) sont présents dans les monocytes, les macrophages et le tissu thymique, ce qui indique un rôle spécifique de la vitamine D et de ses métabolites dans le système immunitaire.(13)
Exercices
L'exercice physique régulier a été associé à un système immunitaire sain. Les activités modérées et de haut niveau favorisent l'état du thymus en réduisant le stress et en améliorant l'organisme dans son ensemble.(14) Cependant, des niveaux trop élevés et constants d'exercice physique sont associés à une augmentation des biomarqueurs liés au vieillissement du système immunitaire, qui sont partiellement réduits avec le vieillissement physiologique.(15)
Réduction du stress
Le stress chronique peut endommager le système immunitaire, y compris le thymus.(16) L'augmentation des taux de glucocorticoïdes (par exemple, le cortisol) peut provoquer l'apoptose des thymocytes.(17) Les méthodes de réduction du stress, y compris la méditation, le yoga, la pleine conscience et bien d'autres encore, dont il est question dans l'ouvrage The Resilient Beingpourraient indirectement aider le thymus à mieux fonctionner.
Traitements hormonaux
Certaines études ont examiné la possibilité d'utiliser les hormones de croissance, les stéroïdes sexuels et les hormones thymiques pour restaurer la fonction thymique, en particulier chez les personnes âgées ou les personnes immunodéprimées. Des études ont montré que l'hormone de croissance (GH), la ghréline (GRL) et le facteur de croissance analogue à l'insuline 1 (IGF-1) peuvent stimuler la régénération du thymus. Dans certains modèles animaux, l'administration de GH ou d'IGF-1 a entraîné une augmentation de la masse thymique et de la production de cellules T. Les essais cliniques chez l'homme ont montré des résultats prometteurs. Des essais cliniques chez l'homme ont montré des résultats prometteurs dans l'utilisation de la GH pour la régénération du thymus.(18-20)
Éviter les substances nocives
Fumer et boire trop d'alcool peut aggraver la réponse immunitaire et donc être préjudiciable au thymus. L'exposition chronique aux pesticides, aux métaux lourds comme le plomb et le mercure, au benzène et à d'autres produits chimiques industriels, l'utilisation à long terme de médicaments immunosuppresseurs ou de corticostéroïdes, les polluants atmosphériques tels que les particules fines (PM2,5) et les drogues récréatives peuvent tous altérer la fonction du thymus.(21-23)
Immunothérapie
Des thérapies avancées telles que les cytokines ou les peptides thymiques sont à l'étude pour améliorer la fonction thymique, en particulier pour des maladies telles que le VIH/SIDA et certains cancers. Parmi ces thérapies, on peut citer le facteur de croissance des kératinocytes (KGF), l'interleukine-22, le RANKL, le facteur de croissance épidermique (EGF), le BMP4 et l'IL-7.(24)
Qualité du sommeil
Le sommeil est essentiel au maintien d'un système immunitaire sain ; sa qualité influence directement la fonction thymique. Le thymus est responsable de la production des lymphocytes T, essentiels à l'immunité adaptative, et son activité est étroitement liée aux rythmes circadiens de l'organisme. Un sommeil de mauvaise qualité, irrégulier ou insuffisant peut perturber ces rythmes, entraînant une diminution de la production de lymphocytes T et une altération des réponses immunitaires.(25)
Pendant le sommeil profond, l'organisme subit des processus réparateurs, notamment la libération d'hormones de croissance et la régulation des marqueurs inflammatoires, ce qui favorise la santé du thymus. À l'inverse, le manque chronique de sommeil peut élever les niveaux de cortisol, supprimant l'activité du thymus et accélérant son involution.(26)
Les peptides et le thymus : Un potentiel futur pour la santé du système immunitaire ?
Les peptides thymiques, en particulier, ont fait l'objet d'une grande attention en raison de leur valeur potentielle pour le bon fonctionnement du thymus et du système immunitaire. Les peptides sont des agents biologiques naturels ou synthétiques utilisés pour moduler l'activité du thymus. Les peptides thymiques synthétiques les plus étudiés sont les suivants :
Thymosine Alpha-1
Le peptide thymique le plus étudié. La thymosine alpha-1 (Tα1) améliore la fonction des cellules T et a été utilisée dans plusieurs contextes cliniques, tels que le traitement des infections virales chroniques, de certains cancers et des déficiences immunitaires. Il s'agit de modifier la réponse immunitaire, d'améliorer la maturation des lymphocytes T et de stimuler la production de cytokines.(27-28) En général, Tα1 peut se lier à TLR3/4/9 et activer les voies de signalisation IRF3 et NF-κB en aval, favorisant ainsi la prolifération et l'activation des cellules immunitaires cibles. En outre, TLR2 et TLR7 (toll-like receptors 2 et 7) sont également associés à Tα1, ce qui renforce les réponses immunitaires innées et adaptatives.(29)
Thymosine Beta-4 (TB-500)
La thymosine bêta-4 (Tβ4) ou TB-500 est un peptide synthétique utilisé aujourd'hui en raison de son rôle crucial dans la cicatrisation des tissus, la régénération et la réparation cellulaire. Il a été étudié pour sa capacité à accélérer le processus de cicatrisation, à réduire l'inflammation et à offrir une protection cardiovasculaire, en particulier après un infarctus du myocarde.(30)
La Tβ4 a diverses activités biologiques, telles que l'inhibition de l'inflammation et de l'apoptose et la promotion de la prolifération et de l'angiogenèse. En outre, des expériences animales et des études cliniques ont montré que le Tβ4 exerce des effets thérapeutiques sur plusieurs maladies ou lésions, telles que l'infarctus du myocarde et les lésions d'ischémie-reperfusion, la fibrose hépatique et rénale, la colite ulcéreuse, le cancer du côlon et les traumatismes cutanés.(31)
Cependant, son utilisation chez l'homme est expérimentale et n'est pas approuvée par la FDA, et la plupart des études sont menées sur des animaux.
Image : Interprétation artistique du TB-500.
Analogues synthétiques de la thymuline
Des analogues synthétiques de la thymuline ont été étudiés pour améliorer sa stabilité et son activité biologique. Ces analogues sont créés pour imiter l'action immuno-modulatrice de la thymuline naturelle, principalement dans la fonction des lymphocytes T et l'effet anti-inflammatoire.(32)
Conclusion
Le thymus joue un rôle essentiel dans la régulation du système immunitaire, principalement par le biais du développement et de la maturation des lymphocytes T. Le thymus se rétrécit naturellement et devient moins actif. Il rétrécit naturellement et devient moins actif avec l'âge, mais il existe des moyens pratiques de le faire fonctionner au mieux. Une alimentation anti-inflammatoire, une activité physique régulière, un sommeil de qualité et la réduction du stress sont des actions simples et quotidiennes qui favorisent la santé du thymus. Les peptides thymiques, les thérapies hormonales et l'immunothérapie offrent des possibilités intéressantes pour stimuler la régénération du thymus et l'immunité. En prenant soin du thymus, vous pouvez favoriser une meilleure santé générale et une meilleure résilience.
Références scientifiques :
- Haynes, B. & Markert, M. & Sempowski, G. & Patel, D. & Hale, L. (2000). The role of the thymus in immune reconstitution in aging, bone marrow transplantation, and HIV-1 infection. Revue annuelle d'immunologie 18 (1): 529–560.
- Adkins, B. et al. (1987). Early events in T-cell maturation. Revue annuelle d'immunologie 5 (1): 325–365.
- Savino, W. & Mendes-da-Cruz, D. & Lepletier, A. & Dardenne, M. (2016). Contrôle hormonal du développement des cellules T dans la santé et la maladie. Nature Reviews Endocrinology 12 (2): 77–89.
- Goldstein, A. et al. (1977). Thymosin alpha1 : isolation and sequence analysis of an immunologically active thymic polypeptide. Actes de l'Académie nationale des sciences 74 (2): 725–729.
- Costantini, C. et al. (2019). Une réévaluation de la thymosine alpha1 dans la thérapie du cancer. Frontiers in Oncology 9: 873.
- Dominari, A. et al. (2020). Thymosin alpha 1 : a comprehensive review of the literature. World Journal of Virology 9 (5): 67–78.
- Harris, C. et al. (1994). Three distinct human thymopoietins are derived from alternatively spliced mRNAs. Proceedings of the National Academy of Sciences (Actes de l'Académie nationale des sciences) 91 (14): 6283–6287.
- Hogquist, K. & Baldwin, T. & Jameson, S. (2005). Central tolerance : learning self-control in the thymus (Tolérance centrale : apprentissage de la maîtrise de soi dans le thymus). Nature Reviews Immunology 5 (10): 772–782.
- Audhya, T. & Scheid, M. & Goldstein, G. (1984). Contrasting biological activities of thymopoietin and splenin, two closely related polypeptide products of thymus and spleen. Proceedings of the National Academy of Sciences 81 (9): 2847–2849.
- Dardenne, M. & Savino, W. & Berrih, S. & Bach, J. (1985). Un épitope dépendant du zinc sur la molécule de thymuline, une hormone thymique. Proceedings of the National Academy of Sciences 82 (20): 7035–7038.
- Taub, D. et Longo, D. (2005). Aperçu du vieillissement et de la régénération du thymus. Immunological Reviews 205 (1): 72–93
- Dardenne, M. (2002). Zinc et fonction immunitaire. European Journal of Clinical Nutrition 56 (3) : S20-S23.
- Maggini, S. & Wintergerst, E. & Beveridge, S. & Hornig, D. (2007). Des vitamines et oligo-éléments sélectionnés soutiennent la fonction immunitaire en renforçant les barrières épithéliales et les réponses immunitaires cellulaires et humorales. British Journal of Nutrition 98 (S1) : S29-S35
- Duggal, N. & Pollock, R. & Lazarus, N. & Harridge, S. & Lord, J. (2018). Les principales caractéristiques de l'immunosénescence, y compris la réduction de la production thymique, sont améliorées par des niveaux élevés d'activité physique à l'âge adulte. Aging Cell 17 (2) : e12750.
- Moro-García, M. et al. (2014). La participation fréquente à des exercices de haut volume tout au long de la vie est associée à une réponse immunitaire adaptative plus différenciée. Cerveau, comportement et immunité 39: 61–74.
- Domínguez-Gerpe, L. & Rey-Méndez, M. (1997). Time-course of the murine lymphoid tissue involution during and following stressor exposure. Sciences de la vie 61 (10): 1019–1027.
- Jondal, M. & Pazirandeh, A. & Okret, S. (2004). Different roles for glucocorticoids in thymocyte homeostasis ? TRENDS in Immunology 25 (11): 595–600.
- Savino, W. & Dardenne, M. (2010). Modulation pléiotropique des fonctions thymiques par l'hormone de croissance : de la physiologie à la thérapie. Opinion actuelle en pharmacologie 10 (4): 434–442.
- Chu, Y. et al (2008). Exogenous insulin-like growth factor 1 enhances thymopoiesis predominantly through thymic epithelial cell expansion. Blood (en anglais) 112 (7): 2836–2846.
- Taub, D. & Murphy, W. & Longo, D. (2010). Rajeunissement du thymus vieillissant : voies de signalisation médiées par l'hormone de croissance et la ghréline. Current Opinion in Pharmacology 10 (4): 408–424.
- Shiels, M. et al. (2014). Cigarette smoking and variations in systemic immune and inflammation markers. Journal of the National Cancer Institute 106 (11) : dju294.
- Han, Y. & Lin, T. L. & Pruett, S. (1993). Thymic atrophy caused by ethanol in a mouse model for binge drinking : involvement of endogenous glucocorticoids. Toxicologie et pharmacologie appliquée 123 (1): 16–25.
- Ustarroz-Cano, M., López-Ángel, M., López-Valdez, N., García-Peláez, I. et Fortoul, T. I. (2019). L'effet de la pollution atmosphérique sur le thymus. Dans Thymus. IntechOpen.
- Duah, M. & Li, L. & Shen, J. & Lan, Q. & Pan, B. & Xu, K. (2021). Dégénérescence et régénération du thymus. Frontiers in Immunology 12: 706244.
- Besedovsky, L. & Lange, T. & Haack, M. (2019). La diaphonie sommeil-immunité dans la santé et la maladie. Physiological Reviews 99 (3): 1325–1380.
- Irwin, M. R., Olmstead, R. et Carroll, J. E. (2016). Sleep disturbance, sleep duration, and inflammation : a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biological psychiatry, 80(1), 40-52.
- Romani, L. et al. (2007). Thymosin α1 : an endogenous regulator of inflammation, immunity, and tolerance (Thymosine α1 : un régulateur endogène de l'inflammation, de l'immunité et de la tolérance). Annales de l'Académie des sciences de New York 1112 (1): 326–338.
- Romani, L. et al. (2012). Jack of all trades : thymosin α1 and its pleiotropy (le valet de tous les métiers : la thymosine α1 et sa pléiotropie). Annales de l'Académie des sciences de New York 1269 (1): 1-6.
- Tao, N. et al. (2023). La thymosine α1 et son rôle dans les maladies infectieuses virales : The Mechanism and Clinical Application. Molecules 28 (8): 3539.
- Maar, K. et al (2021). Utilisation de peptides sécrétés essentiels au développement, tels que la thymosine bêta-4, pour rappeler aux organes adultes leur état embryonnaire - nouvelles orientations dans les thérapies régénératives anti-âge. Cellules 10 (6): 1343.
- Xing, Y. & Ye, Y. & Zuo, H. & Li, Y. (2021). Progrès sur la fonction et l'application de la thymosine β4. Frontiers in Endocrinology 12: 767785.
- Lunin, S. & Khrenov, M. & Novoselova, T. & Parfenyuk, S. & Novoselova, E. (2008). Thymulin, a thymic peptide, prevents the overproduction of pro-inflammatory cytokines and heat shock protein Hsp70 in inflammation-bearing mice. Investigations immunologiques 37 (8): 858–870.





