Pääasiallinen fysiologinen mekanismi, joka vaikuttaa vakauteen ja yleiseen vireystilaan työpäivän aikana, on verensokerin säätely. Verensokerin vakaan tason ylläpitäminen pidättäytymällä ylensyömisestä, jatkuvasta välipalasta ja säännöllisistä aterioista on avain tuottavuuteen ja mielen selkeyteen.
Jatkuvat piikit ja verensokerin romahdukset ovat merkittäviä mielialan vaihteluita. Erityisesti hypoglykemia (matala verensokeri) voi aiheuttaa ahdistusta, ärtyneisyyttä ja ärtyneisyyttä, jota yleensä edeltää merkittävä kognitiivisen suorituskyvyn heikkeneminen . Toisaalta diabeetikoille korkea verensokeri liittyy heikentyneeseen kognitiiviseen suorituskykyyn ja negatiivisiin mielialoihin . Verensokeri voi laskea alhaiselle tasolle jopa terveillä henkilöillä esimerkiksi pitkäaikaisen harjoituksen tai paaston vuoksi.
Nälkäsignaalien aktivoitumista ei välttämättä edeltä hypoglykeeminen (fysiologisesti alhainen) verensokeri – yleensä näläntunne ja ruokahalu laukaistaan verensokerin nopeasta laskusta . Näin ollen verensokerin tasaisen tason ylläpitäminen vähentää näläntunnetta ja auttaa saavuttamaan vakaan vireystilan koko työpäivän ajan.
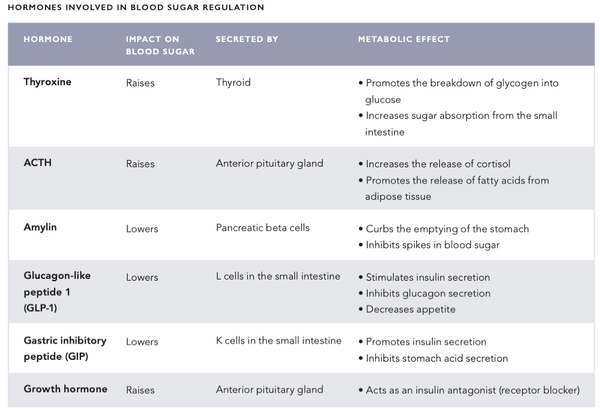
VERENSOKERISÄÄTELYN OSALLISTUVAT HORMONIT
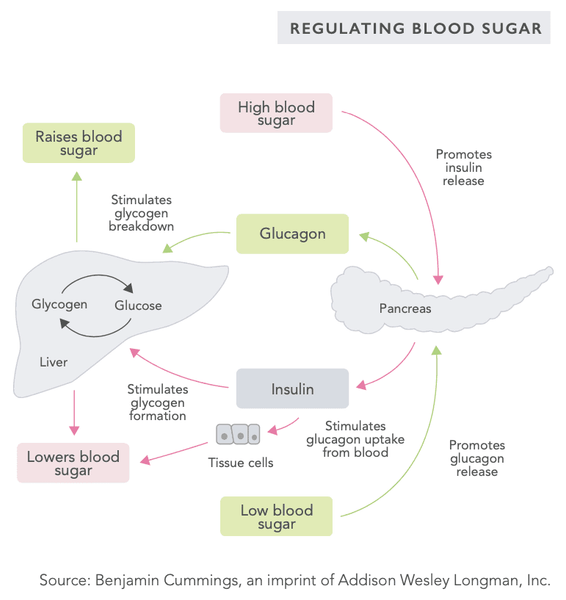
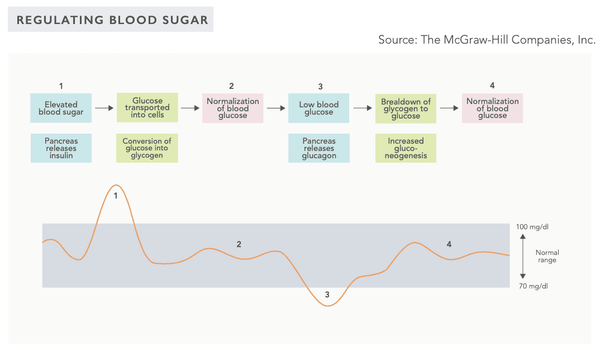
Elimistön verensokerin säätelymekanismi on erittäin kehittynyt järjestelmä , joka sisältää useita sisäelinten erittämiä hormoneja (katso seuraavilla sivuilla oleva taulukko). Verensokeritasoa säätelee negatiivinen palautejärjestelmä – tämä järjestelmä pyrkii saattamaan kehon systeemisen homeostaasin tilaan eli tasapainotilaan.
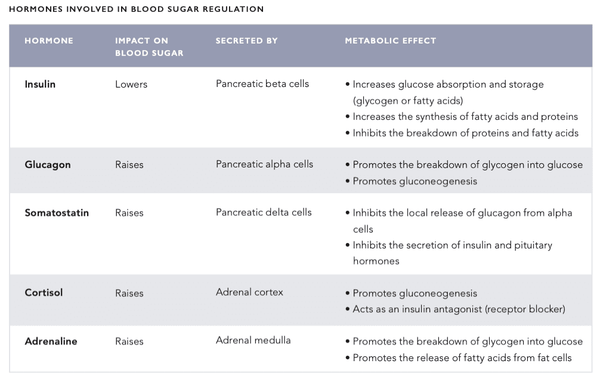
Kun verensokeritaso on korkea, verenkiertoon erittyy hormonien, kuten insuliinin pulsaatioita, jotka alentavat verensokeritasoa . Päinvastoin, kun verensokeritaso on alhainen, glukagonia ja muita hormoneja erittyy verenkiertoon nostamaan verensokeritasoa.
Systeeminen verensokeritason seuranta tapahtuu haiman Langerhansin saarekkeiden beetasoluissa sekä aivojen hypotalamuksen glukoosia tunnistavissa hermosoluissa .
GLYKOLYYSI
Glykolyysi on yksinkertainen osa glukoosin aineenvaihduntaa, jossa glukoosi hajoaa pyruvaaiksi tai laktaatiksi. Energiantuotannon lisäksi glykolyysi säätelee insuliinin eritystä ja liittyy glukoosin stimuloimaan insuliinin eritykseen haiman beetasoluissa. Tällaisissa tapauksissa glukokinaasientsyymin, joka hajottaa glukoosin glukoosi-6-fosfaatiksi, eritys lisääntyy merkittävästi. Koska glukokinaasin aktiivisuus liittyy vahvasti verensokeritasoihin ja siten insuliinin eritykseen, glukokinaasia pidetään pääasiallisena verensokeritason anturina .
glukoneogeneesi
Glukoneogeneesi on aineenvaihduntaprosessi, jossa glukoosia tuotetaan maitohaposta, glyserolista, alaniinista ja glutamiinista. Glukoneogeneesi aktivoituu erityisesti silloin, kun ruokavaliosta puuttuu hiilihydraatteja. Sen avulla elimistö voi myös stabiloida verensokeritason, jos se laskee liian alhaiseksi.
Glukoneogeneesi tapahtuu pääasiassa maksassa (alaniini) ja munuaisten kapseleissa (glutamiini) ja uusimpien tutkimusten mukaan myös suolistossa (erityisesti ohutsuolessa ).
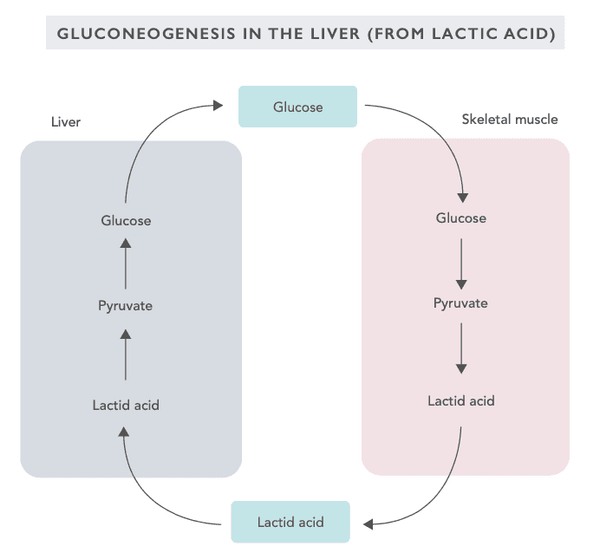
Glukoneogeneesi aktivoituu, kun henkilö on nälkätilassa, noudattaa vähähiilihydraattista ruokavaliota, harjoittaa intensiivistä liikuntaa tai paastoaa. Suurin osa glukoneogeneesin biokemiallisista reaktioista on päinvastainen verrattuna glykolyysin reaktioihin . Glukoneogeneesin entsymaattisia reaktioita säätelee haiman erittämä glukagonihormoni.
GLYKOGENI
Glykogeeni on suurikokoinen molekyyli, joka muodostuu useista (jopa 30 000) glukoosimolekyyleistä. Glykogeenia varastoituu maksaan (10 % painosta), lihassoluihin (2 % painosta) ja vähäisemmässä määrin punasoluihin . Glykoosin lisäksi glykogeeni sitoo kolminkertaisen määrän vettä. Tästä johtuen ihmisen paino voi vaihdella useita kiloja 24 tunnin sisällä riippuen glykogeenivarantojen täyttöasteesta.
Maksan glykogeenivarasto toimii energiavarastona koko kehon ja erityisesti keskushermoston energiantuotannon tarpeisiin. Lihasten glykogeenivarastoa käytetään vain lihassolujen energiantuotantoon . Glykogeenin määrä määräytyy fyysisen harjoituksen, perusaineenvaihdunnan ja ruokailutottumusten perusteella.
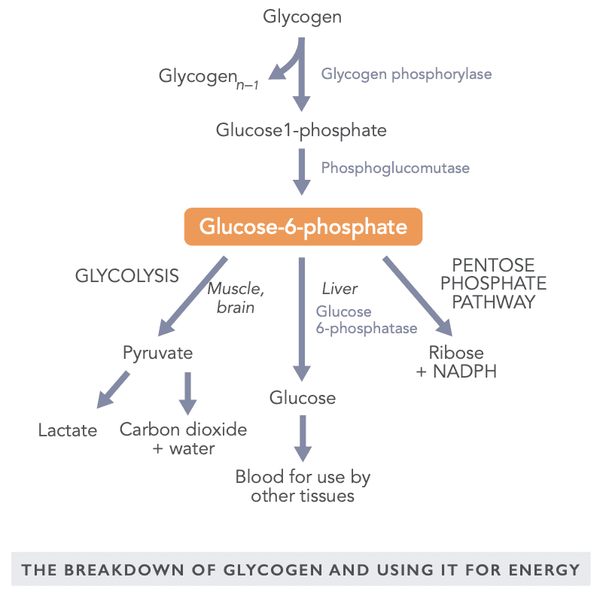
Glykogeenivarastot ovat erityisen tärkeitä verensokerin säätelyssä aterioiden välillä ja intensiivisen harjoittelun aikana. Glukoosia voidaan käyttää energiana myös anaerobisissa olosuhteissa. Toisaalta rasvahapot hajoavat energiaksi vain aerobisissa olosuhteissa. Aivot tarvitsevat tasaisen glukoositason, vaikka ne pystyvät hyödyntämään esimerkiksi maksan paaston aikana tuottamia ketoaineita .
Metabolisesti aktiivinen glykogeenin hajoamistuote on glukoosi-6-fosfaatti, jossa glukoosimolekyyli sitoutuu yhteen fosfaattiryhmään . Sitä voidaan käyttää lihaksen energialähteenä joko aerobisissa tai anaerobisissa olosuhteissa, hyödyntää maksan kautta glukoosina muualla kehossa tai muuntaa riboosiksi ja NADPH:ksi käytettäväksi eri kudoksissa (esimerkiksi lisämunuaisessa, punasoluissa, rintamaidossa) rauhaset ja maksan rasvasolut).
VERENSOKERITASOA SÄÄTELYTTÄVÄT RUOKA- JA LISÄLISÄT
Erilaisten elintarvikkeiden vaikutukset verensokeriin on perinteisesti kuvattu glykeemisen indeksin (GI) avulla. Se edustaa ruoan aiheuttamaa verensokerin muutosta vertailuarvoon (glukoosiliuos) verrattuna. Toisaalta glykeeminen kuormitus (GL) osoittaa aterian kokonaisvaikutuksen verensokeriin. GI- ja GL-käsitteet kehitettiin alun perin diabeetikoille. Niitä on myös yritetty soveltaa muiden terveysongelmien (kuten syövän ja sydänsairauksien) hoidossa ristiriitaisin tuloksin. GI- ja GL-arvoja on kritisoitu siitä, että ne eivät ota huomioon ruoan aiheuttamaa yksilöllistä vaihtelua ja insuliinivastetta. Myöskään eri ainesosista koostuvan aterian laukaisemaa glykeemistä vastetta ei voida luotettavasti arvioida.
Insuliiniindeksi on kuitenkin kehitetty kuvaamaan parhaiten ruoan vaikutusta insuliinin erittymiseen . Toistaiseksi insuliiniindeksiin on kiinnitetty vain vähän huomiota, vaikka se näyttää olevan hyödyllinen tyypin 1 diabeetikoille , jotka ovat aiemmin tottuneet arvioimaan ja laskemaan ravinnon sisältämien hiilihydraattien määrää. Kylläisyyden pistemäärää voidaan käyttää yhdessä insuliiniindeksin kanssa . Se edustaa tietyn ruoan tuomaa kylläisyyden tunnetta. Esimerkiksi perunoiden insuliiniindeksi on korkea, 121, mutta myös niiden kylläisyyspiste on erittäin korkea, 323 (katso lisätietoa seuraavien sivujen taulukosta).
Matalan GI:n ruokavaliota suositellaan usein painonpudotukseen keskittyville henkilöille. Pelkästään glykeemisellä indeksillä näyttää kuitenkin olevan vain vähän vaikutusta painonpudotukseen verrattuna muihin samankalorisiin ruokavalioihin .
Tutkimusten mukaan ruokavalioon, jossa on jatkuvasti korkea glykeeminen kuormitus, liittyy korkeampi hiljainen tulehdus . Sitä vastoin Välimeren ruokavalio, jossa on alhainen glykeeminen kuormitus, on varsin tehokas lihavuuden, insuliiniresistenssin, korkean verenpaineen ja korkean kolesterolin vähentämisessä, ainakin metabolisesta oireyhtymästä kärsivillä naisilla yhden tutkimuksen mukaan.
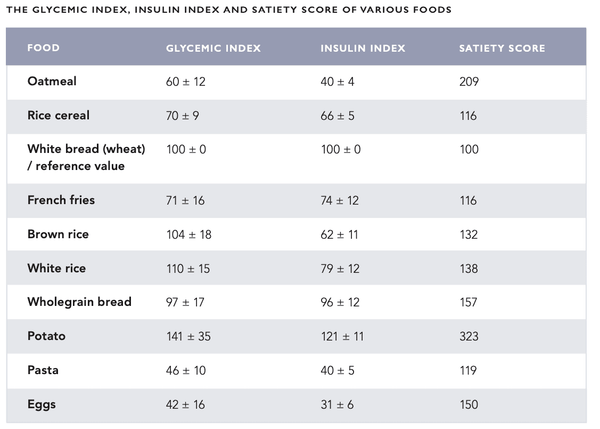
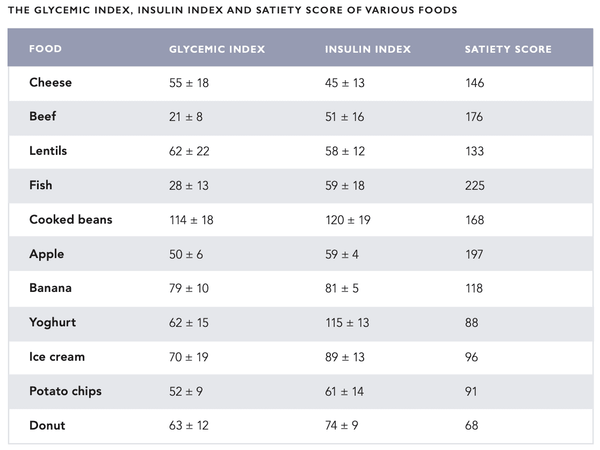
Ruokavalio, jossa on melko alhainen glykeeminen kuormitus ja insuliiniindeksi, on edullinen vaihtoehto sekä terveydelle että henkiselle vireydelle. Liikunnan jälkeen tulee syödä korkean insuliiniindeksin omaavia ruokia lihasten ja maksan glykogeenivarantojen täydentämiseksi insuliinilla.
Aterian aiheuttamaa verensokerin piikkiä voidaan tasapainottaa erilaisilla elintarvikkeilla ja lisäravinteilla (katso seuraavat luvut). Länsimaissa kanelia lisätään tyypillisesti makeisiin jälkiruokiin ja leivonnaisiin, jotka nostavat merkittävästi verensokeria. Kiinassa lääkesieniä ja yrttejä
sisällytetään ruokavalioon niiden verensokeria tasapainottavien ominaisuuksiensa vuoksi. Intian Ayurvedic-lääketiede sisältää useita verensokeria tasapainottavia yrttejä, kuten Gymnema Sylvestre. Hindinkielinen sana "gurmar" tarkoittaa "sokerin tuhoajaa" .
VERESOKERIN SÄÄTÖ RUOKALLA
Kaneli on mauste, joka on johdettu Cinnamomum-suvun kasveista. Euroopassa myytävä kaneli on yleensä kiinalaista (cassia) kanelia (Cinnamomum cassia, Cinnamomum aromaticum), joka sisältää kumariinia, joka on myrkyllistä maksalle ja munuaisille suurina määrinä kulutettuna ( katso lisätietoa Biohacker's Handbookin ravitsemusluvusta ).
Maailmassa on lukuisia kanelin lajikkeita, joiden kumariinipitoisuus vaihtelee huomattavasti. Kanelin nauttiminen teenä on perinteinen tapa käyttää sitä. Tämä menetelmä vähentää myös merkittävästi kumariinin saantia. Kumariinin toksisuus vaihtelee yksilöiden välillä. Se liittyy geneettisen muunnelman CYP2A6 kykyyn toimia osana maksan sytokromi P450 -järjestelmää .
Kanelin verensokeria ja insuliiniherkkyyttä säätelevät ominaisuudet liittyvät vahvasti sen korkeaan kromipitoisuuteen sekä polyfenolien ja haihtuvien polymeerien vaikutuksiin . Tutkimussuunnitelmasta ja käytetystä annoksesta riippuen kaneli alentaa paastoverensokeria 10–29 % . Tyypillinen suositeltu päiväannos on 1-6 grammaa . Kun päätät käytettävästä määrästä, on suositeltavaa ottaa huomioon geneettinen taustasi (CYP2A6-polymorfismi), tavoitteesi ja mahdolliset yhteisvaikutukset lääkevalmisteiden kanssa.
Monien suorituskykyä lisäävien yrttien ja niin sanottujen älylääkkeiden vaikutukset liittyvät usein myös verensokerin säätelyyn. Esimerkiksi vuonna 2014 tehdyn meta-analyysin mukaan ginseng-juuren on havaittu auttavan alentamaan paastoverensokeritasoja .
Ruoat ja mausteet, jotka auttavat tasapainottamaan verensokeria:
- Kaneli
- Mustikka
- Valkosipuli
- Hapankirsikka
- Omenaviinietikka
- Kahvia
- Chia
- Kumina
- Inkivääri
- Shiitake sieni
- Sitruuna
- Kurkuma
- Kaakao (ja tumma suklaa)
Lisäravinteet ja lääkkeet, jotka auttavat tasapainottamaan verensokeria:
- Kromi
- D-vitamiini
- Alfa-lipoiinihappo
- Reishi
- Maitake
- Chaga
- Cordyceps
- Psyllium
- MCT öljy
- Gymnema sylvestre
- Karvas meloni
- Viikukkakktus
- sarviapila
- Purslane
- Banaban lehtiä
- Maitoohdake
- Resveratroli
- Magnesium
- Panax ginseng
- Berberiini
- Vihreä tee
- Korianteri
- Vanadyylisulfaatti
VERENSOKERI TASAPAINOINTI
Kulutettava n. 30 minuuttia ennen korkeahiilihydraattista ateriaa:
- 100-300 mg alfa-lipoiinihappoa
- 50-100 mg kromia
- 500–1000 mg berberiiniä tai 100–200 mg dihydroberberiiniä
- 200-400 mg EGCG:tä (vihreän teen uute)
- 50 mg resveratrolia
- 100 mg magnesiummalaattia
KAHVIN VAIKUTUS VERENSOKERISÄÄTELYN
Pitkäaikaiset tutkimukset ovat löytäneet yhteyden kahvin kulutuksen ja korkeamman insuliiniherkkyyden välillä sekä pienentyneen riskin sairastua tyypin 2 diabetekseen ( katso lisätietoja Biohacker's Handbookin ravitsemusluvun osiosta "Kahvi" ). Näistä löydöistä huolimatta kahvi voi alentaa äkillisesti insuliiniherkkyyttä ja nostaa verensokeritasoja henkilöillä, jotka eivät ole tottuneet kofeiiniin .
Kahvin aiheuttamat muutokset verensokerin säätelyssä johtuvat mitä todennäköisimmin kofeiinista . Kofeiinittoman kahvin ei ole havaittu aiheuttavan samanlaista heilahtelua verensokeritasoissa. Vaikuttaa siltä, että säännöllinen kahvin kulutus vähentää myös kahvin vaikutuksia verensokeriin .
Yksilöt, joilla on pistemutaatio CYP1A2-geenissä (muunnelma 164A>C), hajottavat kofeiinia huomattavasti hitaammin kuin yleinen väestö. Tämä liittyy myös kahvin aiheuttamiin verensokerivaihteluihin sekä korkeampiin paastoverensokeritasoihin , erityisesti henkilöillä, joilla on korkea verenpaine.
Useimmille ihmisille kohtuullinen kahvinkulutus (3–4 kuppia päivässä) sopii yhteen terveellisen, tasapainoisen ruokavalion ja aktiivisen elämäntavan kanssa . Kattavan meta-analyysin mukaan kohtuullinen kahvin kulutus voi pidentää elinikää, alentaa riskiä sairastua tyypin 2 diabetekseen ja sydän- ja verisuonisairauksiin sekä ehkäistä ennenaikaista kuolemaa näihin sairauksiin . Kahvin terveyshyödyt johtuvat todennäköisesti antioksidanteista. se sisältää, kuten polyfenoleja. Kahvista on tosiaankin löydetty yli 1000 antioksidanttiyhdistettä, jopa enemmän kuin vihreästä teestä ja kaakaosta .
UNI- JA VERENSOKERISÄÄTELY
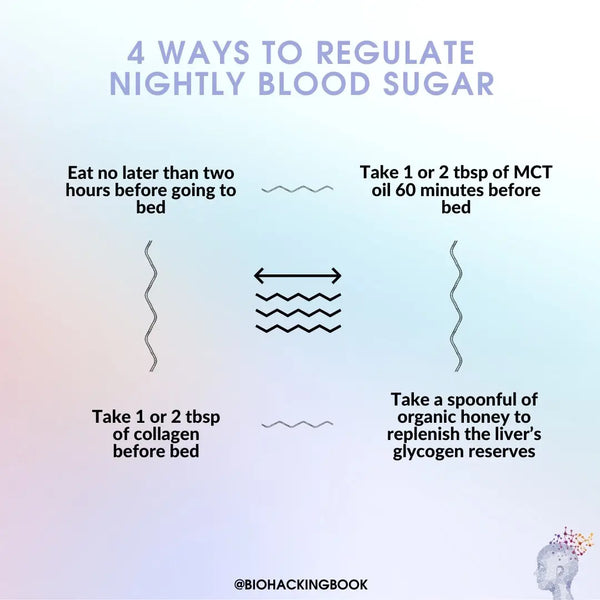
Verensokeritaso laskee tasaisesti paastottaessa valveillaoloaikana. Toisaalta verensokeritasot pysyvät yleensä vakiona unen aikana . Tämä johtuu siitä, että verensokeritaso nousee aluksi noin 20 % unisyklin alussa ja laskee sitten hitaasti normaalille tasolle . Nämä havainnot osoittavat, että glukoosin energiakäyttö vähenee unen aikana. Ei-REM-unen aikana aivojen glukoosiaineenvaihdunta heikkenee 11 % . Sitä vastoin glukoosiaineenvaihdunta kiihtyy REM-unen ja hereillä ollessa .
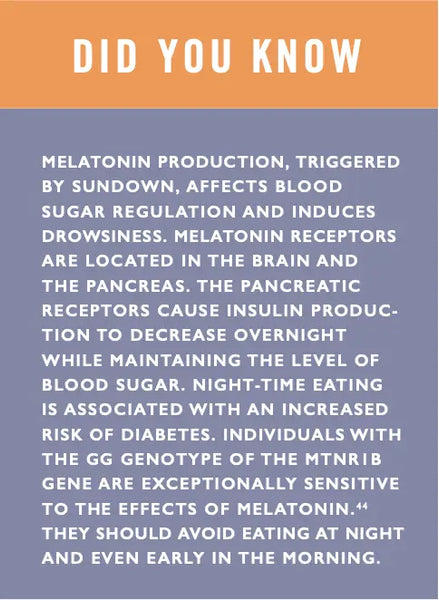
Unenpuute vaikuttaa merkittävästi verensokerin säätelyyn . Vaikea unenpuute (neljä tuntia unta yössä) jo yhden viikon ajan heikentää glukoosin käyttöä energiana ja nostaa paastoverensokeria . Se on myös altistava tekijä sokeriaineenvaihdunnan häiriöille (esidiabetekselle). Tutkimuksen mukaan henkilöillä, jotka nukkuvat alle 6,5 tuntia yössä, on jopa 40 % pienempi insuliiniherkkyys verrattuna niihin, jotka nukkuvat normaalisti (7–8 tuntia) yössä . Heikentynyt insuliiniherkkyys on altistava tekijä verensokerivaihteluille, liikalihavuudelle ja tyypin 2 diabetekselle. Vuonna 2015 julkaistun meta-analyysin mukaan verensokerin säätelyssä ja diabeteksen ehkäisyssä optimaalinen päiväunen määrä on 7–8 tuntia. On syytä huomata, että liiallinen uni voi myös heikentää verensokerin säätelyä .
Unenpuute häiritsee myös nälän tunnetta vaikuttamalla leptiinin ja greliinin erittymiseen. Nuorilla miehillä tehdyn tutkimuksen mukaan riittämätön uni (4 tuntia) vain kahtena peräkkäisenä yönä alensi kylläisyyshormonin leptiinin tasoa 18 % ja nosti nälkähormonin greliinin tasoa 28 %. Univajetta kokeneet henkilöt ilmoittivat ruokahalun merkittävästä (24 %) lisääntymisestä erityisesti makeiden, suolaisten tai tärkkelyspitoisten ruokien suhteen. Myös kattavammat väestötutkimukset ovat tuottaneet vertailukelpoisia tuloksia .
Lue kattava artikkeli syvän unen optimoinnista ja unen laadun parantamisesta täältä.
TASAPOIDA VERENSOKERITASOSI HELPOSTI AJATTAISELLA PAASTOSSA
Jaksottaisella paastolla tarkoitetaan paastoamista merkittävän osan vuorokaudesta (esimerkiksi 16 tuntia) ja päivittäisen ravinnon nauttimista jäljellä olevan ruokailuikkunan aikana (esim. 8 tuntia). Yksinkertaisin tapa toteuttaa tämä on pidentää yön paastoa jättämällä väliin aamiainen ja nauttimalla päivän ensimmäisestä ateriasta iltapäivällä.
Jaksottaisen paaston käsite vastustaa tämän päivän elintarviketeollisuuden ja kuntoilukulttuurin edistämää "kuuden pientä ateriaa päivässä" -trendiä. Laiduntamista rationalisoidaan usein väitteillä aineenvaihdunnan aktivoimisesta ja painonhallinnan helpottamisesta. Tällaisille väitteille ei kuitenkaan ole löydetty tieteellistä perustaa . Itse asiassa perusaineenvaihduntanopeus (BMR) kasvaa hieman 36 tunnin paaston jälkeen – vasta 72 tunnin kuluttua BMR alkaa hitaasti laskea.
Jaksottainen paasto auttaa saavuttamaan halutun kalorirajoituksen, kun tavoitteena on kuona-aineiden poistaminen kehosta (autofagia) tai laihtuminen. Parannuksia sokeriaineenvaihdunnan säätelyssä on raportoitu myös ajoittaisen paaston yhteydessä.
Erään tutkimuksen mukaan usein (6 kertaa päivässä) syöneiden ihmisten energiankulutuksessa ei ollut merkittäviä eroja harvemmin (2 kertaa päivässä) syöviin verrattuna. Samassa tutkimuksessa havaittiin, että aamupaastonneet söivät luonnollisesti hieman vähemmän ja söivät myös hieman vähemmän hiilihydraatteja .
Evoluutionäkökulmasta katsottuna ihminen kehittyi syömään silloin, kun ruokaa on saatavilla (yleensä illalla) – loppuaika kului ruoan hankkimiseen (aamulla ja päivällä).
Käytännössä jaksottainen paasto toimii hyvin, koska se mahdollistaa tyydyttävien aterioiden nauttimisen ruokailuikkunan aikana samalla kun kokonaisenergian saanti pysyy kohtuullisena. Esimerkiksi ruuan (erityisesti hiilihydraattien) nauttiminen iltaisin alentaa merkittävästi stressihormonien tasoa ja edistää unta sekä stabiloi leptiinin, greliinin ja adiponektiinin (rasvanpolttoa) eritystä . Aterioiden nauttiminen myöhemmin illalla aktivoi myös parasympaattista hermostoa, rauhoittaa kehoa ja helpottaa nukahtamista.
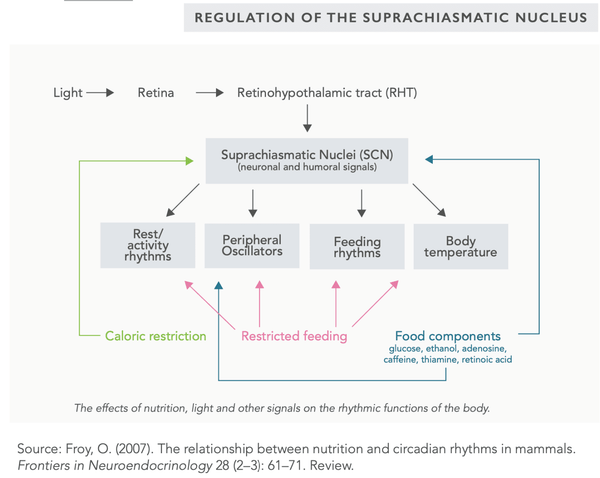
Jaksottaista paastoa (ja kalorirajoitusta) voidaan myös käyttää tasapainottamaan suprakiasmaattisen ytimen (SCN) toimintaa, joka säätelee kehon vuorokausirytmiä . Ensisijainen tekijä SCN:n säätelyssä on valo (erityisesti auringonvalo).
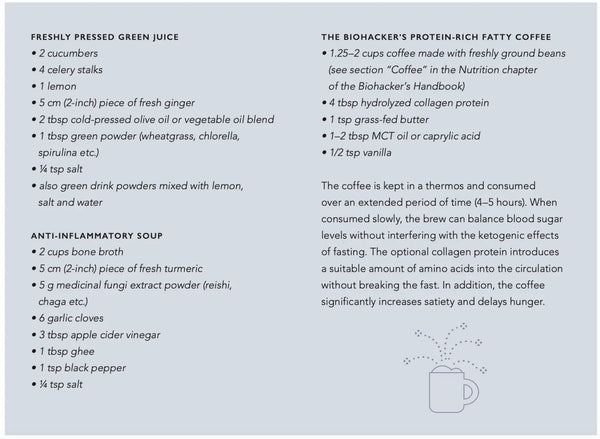
Vettä, teetä, kahvia ja kivennäisvettä kulutetaan usein nestetasapainon ylläpitämiseksi paaston aikana. Vähäenergiaiset vihreät mehut ovat myös hyvä vaihtoehto, koska ne sisältävät välttämättömiä mikroravinteita (katso reseptit seuraavalta sivulta). Erittäin aktiiviset tai urheilulliset ihmiset voivat myös kuluttaa välttämättömiä aminohappoja (EAA) tablettien tai jauheiden muodossa palautumisen maksimoimiseksi .
Jaksottaista paastoa (tai paastoa yleensä) ei yleensä suositella alle 18-vuotiaille, raskaana oleville, imettäville, erittäin väsyneille tai kroonisesta väsymysoireyhtymästä kärsiville henkilöille.
Jaksottaiseen paastoon on erilaisia menetelmiä:
- 24 tunnin paasto 1–2 kertaa viikossa ("Eat Stop Eat")
- 20 tunnin paasto, jota seuraa 4 tunnin ruokailuikkuna ("The Warrior Diet")
- 36 tunnin paasto, jota seuraa 12 tunnin ruokailuikkuna ("Alternate Day Fast")
- 16 tunnin paasto, jota seuraa 8 tunnin ruokailuikkuna ("Leangains")
- 18 tunnin paasto (rasvainen kahvi sallittu), jota seuraa 6 tunnin ruokailuikkuna ("Buletproof Intermittent Fasting")
Paaston / ajoittaisen paaston terveyshyötyjä ovat :
- Voi pidentää elinikää hidastamalla ikääntymisprosessia
- Voi vähentää riskiä sairastua aineenvaihdunta- ja kroonisiin sairauksiin, kuten
- Syöpä
- Dabetes
- Metabolinen oireyhtymä
- Niveltulehdus
- Neurodegeneratiiviset sairaudet (kuten Alzheimerin tauti)
- Voi parantaa insuliiniherkkyyttä ja alentaa verenpainetta
- Voi vähentää oksidatiivista stressiä kehossa
- Voi parantaa kehon hormonitasapainoa
BIOHACKERIN OPAS JAKSIPAASTOON
Jokaisella Biohacker's Handbookin kirjoittajilla on oma katkonaista paastoamista koskeva mallinsa, joka on kehittynyt eri kokeilujen aikana.
Tässä on esimerkkimalli fyysisesti aktiiviselle ja toimistossa työskentelevälle henkilölle:
- Paasto yön yli ja ensimmäisen aterian lykkääminen mahdollisimman paljon (yleensä joskus klo 15.00-18.00 edellisen aterian ajoituksesta riippuen)
- Paaston aikana juo runsaasti nesteitä, kuten kivennäisvettä (runsaasti kivennäisaineita, viivyttää näläntunnetta)
- Nälkä voi viivästyä entisestään ennen ensimmäistä ateriaa syömällä runsaasti kuitua ja suhteellisen vähän energiaa sisältävää omenaa (< 50 kcal) – kurkun syöminen voi myös viivästyttää nälän tunnetta (vähäinen kalorien saanti)
- Harkitse seuraavia vähähiilihydraattisten juomien reseptejä alla (kuva)
- Ensimmäisen aterian tulisi koostua pääasiassa proteiineista, kuitupitoisista vihanneksista ja rasvasta sekä pienestä määrästä hiilihydraatteja (jos halutaan)
- Toisella (ja viimeisellä) aterialla, joka nautitaan klo 20.00-23.00, tulee sisältää runsaasti hiilihydraatteja sekä sopivat määrät rasvaa ja proteiinia – kun se syödään lähellä nukkumaanmenoa, se voi auttaa optimoimaan unen.
- Liikunta ajoitetaan usein joko paastoajan loppuun iltapäivällä tai ensimmäisen aterian jälkeen myöhemmin illalla
Insuliiniherkkyyttä parantavia elämäntapavalintoja ovat mm.
- Riittävän unen saaminen
-
Säännöllinen harjoittelu (erityisesti voimaharjoittelu ja korkean intensiteetin harjoittelu)
- Aerobisen harjoittelun ja voimaharjoittelun yhdistäminen on tehokkain tapa parantaa insuliiniherkkyyttä
- Stressin hallinta ja stressin vähentäminen
- Painonpudotus (erityisesti vyötärön ympärillä)
- Liukoisten kuitujen runsas saanti ruoasta
- Syö enemmän värikkäitä vihanneksia, marjoja ja hedelmiä (erityisesti tummia marjoja, kuten mustikoita ja mustaherukoita)
-
Yrttien ja mausteiden käyttö ruoanlaitossa
-
Kurkuma
-
Inkivääri
-
Kaneli
- Valkosipuli
- Ginseng
- sarviapila
- Lääkesienet (reishi, shiitake, maitake, chaga, cordyceps)
- Omenaviinietikka
- Vihreä tee
-
Hiilihydraattien, erityisesti sokereiden, saannin vähentäminen
-
Säännöllinen paasto ja ajoittainen paasto
-
Liiallisen istumisen välttäminen
-
Prosessoitujen kasviöljyjen ja transrasvojen poistaminen ruokavaliosta
-
Tietyt ravintolisät voivat parantaa insuliiniherkkyyttä:
- Kromi
- Magnesium
- Berberiini
- Resveratroli
- Alfa-lipoiinihappo
VERENSOKERITASON MITTAUS JA SEURANTA
Tasainen verensokeritaso on yksi avaintekijöistä hyvän suorituskyvyn ja henkisen vireyden ylläpitämisessä. Diabeetikoille verensokeritason seuranta on elintärkeää terveyden kannalta. Oman verensokerin seuranta voi olla hyödyllistä myös diabeetikoille – kuten uteliaille biohakkereille, jotka haluavat selvittää, mitkä ravinnon ja elämäntavan tekijät vaikuttavat suorituskykyyn ja henkiseen vireyteen.
Verensokerin testiliuskat otettiin käyttöön 1970-luvulla. Pian niitä seurasivat laitteet, jotka antoivat verensokeriarvon testiliuskojen avulla. Nykyään on mahdollista ottaa nopea sormenpäänäyte ja saada laite analysoimaan se lähes välittömästi. Verensokerin mittaamiseen suunniteltuja oheislaitteita ja sovelluksia on saatavilla myös älypuhelimiin.
Diabeetikot voivat nyt käyttää ihon alle sijoitettuja monitoreja, jotka mittaavat verensokeria lähes jatkuvasti (esim. viiden minuutin välein) . Nämä näytöt varoittavat käyttäjää, kun tulokset ovat liian alhaisia tai korkeita tai kun verensokerissa havaitaan äkillisiä heilahteluja. Tällaisilla laitteilla on mahdollista kerätä pitkäaikaisia verensokeritietoja.
Uusin edistysaskel on laite, joka käyttää laseria (keskiaallonpituuden infrapuna) verensokerin mittaamiseen ilman neulanpistoa . Kehittäjien tekemän tutkimuksen mukaan laitteen tarkkuus on 84 % verikokeeseen verrattuna . Myös erilaisia nanoteknologiaan perustuvia laitteita on kehitteillä.
Verensokerin mittausmenetelmät kehitteillä :
- Piilolinssit , jotka mittaavat verensokeria
- Infrapuna- ja ultraäänilaitteet
- Raman-spektroskopia
- Kertakäyttöiset nanobiosensorit ( verensokerianalyysi syljestä ) ja implantit ( verensokerianalyysi verestä )
- Affiniteettianturit, jotka mittaavat optisesti
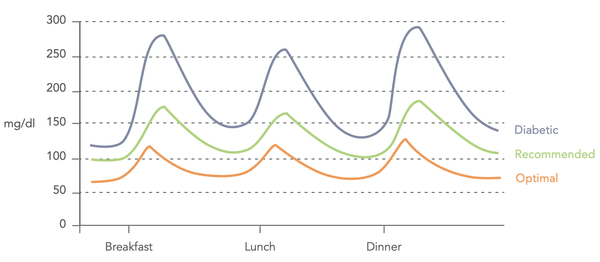 Kuva: Verensokeritasojen vaihtelut (Biohacker's Handbook, 2019).
Kuva: Verensokeritasojen vaihtelut (Biohacker's Handbook, 2019).
VERENSOKERIMITTAUSTEN TULKINTA
Seuraavat suositellut arvot perustuvat useisiin tutkimuksiin . Niitä voidaan käyttää määrittämään optimaaliset arviot pienimmästä mahdollisesta diabeteksen , sydän- ja verisuonitautien , aivohalvauksen , metabolisen oireyhtymän jne. riskistä.
Verensokeriarvoja mitattaessa tulee ottaa huomioon välittömästi edeltävä ruokailu. Esimerkiksi henkilöillä, jotka noudattavat vähähiilihydraattista ruokavaliota, on yleensä alentunut sokerinsietokyky, mikä voi aiheuttaa korkeita mittausarvoja runsaan hiilihydraattisen aterian jälkeen. Tämä tulee ottaa huomioon suoritettaessa oraalinen glukoosialtistustesti laboratorioympäristössä. Suositeltu sopeutumisaika on neljä päivää ennen testiä, jonka aikana hiilihydraatteja tulee kuluttaa vähintään 150 g päivässä.
-
Paastoverensokeri (paastoplasman glukoosi, FPG)
- Normaali: 4–6 mmol/l tai 72–108 mg/dl
- Optimaalinen: 4,0–5,3 mmol/l tai 72–95 mg/dl ( Life Extension Foundation suosittelee 4,0–4,7 mmol/l tai 72–85 mg/dl)
- Glykoitu hemoglobiini (HbA1C)
- Normaali: 20–42 mmol/L / 4,0 % – 6,0 %
- Optimaalinen: 20–34 mmol/L / 4,0 % – 5,3 %
- Häiritseviä tekijöitä voivat olla anemia (liian alhainen tulos) tai nestehukka (liian korkea tulos)
- Suun kautta otettava glukoositoleranssitesti (OGTT)
- Otetut arvot: paastoverensokeri ja verensokeri
- 1 tunti ja 2 tuntia glukoosialtistuksen (75 g) jälkeen
- Normaaliarvo 1 tunnin kohdalla: < 10,0 mmol/l tai 180 mg/dL Optimaalinen arvo: < 7,8 mmol/l tai 140 mg/dl
- Normaaliarvo 2 tunnin kuluttua: < 8,6 mmol/l tai 155 mg/dL Optimaalinen arvo: < 6,7 mmol/l tai 121 mg/dl
- Verensokeritason mittaaminen 1 tunnin ja 2 tunnin kuluttua aterian jälkeen
- Verensokeritasojen itseseuranta 24 tunnin aikana (huomaa, että kotikäyttöön tarkoitettua monitoria käytettäessä virhemarginaali on noin 10 %)
- Paastoverensokeri 12 tunnin paaston jälkeen
- Verensokeri juuri ennen lounasta
- Verensokeri tunti lounaan jälkeen (optimaalinen arvo < 7,8 mmol/l) tai 140 mg/dl
- Verensokeri 2 tuntia lounaan jälkeen (optimaalinen arvo < 6,7 mmol/l) tai 121 mg/dl
- Verensokeri 3 tuntia lounaan jälkeen (optimaalinen arvo < 5,3 mmol/L) tai 95 mg/dl
Jos haluat oppia tulkitsemaan omia verensokeriarvojasi ja ennen kaikkea mitä voit tehdä verensokeritasosi tasapainottamiseksi, suosittelemme Optimize Your Lab Results -verkkokurssin suorittamista. Alla on lisämateriaalia kurssilta mm. insuliinin mittaamiseen ja insuliiniherkkyyden arviointiin.
PAASTOINSULIINI
Insuliini on hormoni, jota haiman beetasolut tuottavat ja erittävät. Elimistö erittää insuliinia vasteena syömisen aiheuttamiin kohonneisiin verensokeritasoihin tai lisääntyneen stressin aiheuttamaan kortisolin erittymiseen. Insuliini lisää glukoosin imeytymistä ja varastointia sekä rasvahappojen ja proteiinien synteesiä ja estää proteiinien ja rasvahappojen hajoamista. Korkeaa insuliinitasoa esiintyy insuliiniresistenssin, liikalihavuuden, metabolisen oireyhtymän, insulinooman, Cushingin oireyhtymän tai liiallisten insuliini- tai kortikosteroidiannosten yhteydessä. Alhaisia insuliinitasoja esiintyy diabeteksen, hypopituitarismin ja erilaisten haimasairauksien yhteydessä. Ihannetapauksessa paastoinsuliinitason tulisi olla vertailualueen alimmalla tasolla .
Insuliini estää lipolyysiä eli rasvan hajoamista energiaksi. Jos kehon varastoituneet insuliinitasot ovat jatkuvasti koholla, veressä kiertävät rasvahapot varastoituvat rasvakudokseen. Tätä kutsutaan lipogeneesiksi. Erityisesti korkea verensokeritaso ja hiilihydraattirikas ruokavalio stimuloivat insuliinin eritystä. Runsas proteiinin saanti lisää myös insuliinin eritystä . Näistä tekijöistä johtuen paastoinsuliinitason tulisi olla melko alhainen, vertailualueen alemmalla puoliskolla. Korkeat insuliinitasot voivat myös olla altistava tekijä kroonisille sairauksille, joita käsitellään HbA1C-arvon kuvauksessa.
- Vertailualue : 2,0–20 mIU/L
HOMA-IR (INSULIINIHERKKYYS)
Laskemalla paastoglukoosin ja paastoinsuliinin välistä vuorovaikutusta voidaan arvioida haiman beetasolujen toimintaa ja kehon insuliiniherkkyyttä. Insuliiniherkkyys riippuu siitä, kuinka paljon insuliinia on eritettävä tietyn glukoosimäärän varastoimiseksi. Insuliiniherkkyys on olemassa, kun vain pieni määrä insuliinia tarvitaan varastoimaan tietty määrä glukoosia soluihin. Sitä vastoin insuliiniresistenssi on olemassa, kun tarvitaan enemmän insuliinia vastaavan glukoosimäärän varastoimiseen.
Insuliiniresistenssi ja alhainen insuliiniherkkyys voivat johtaa tyypin 2 diabetekseen, alkoholittomaan rasvamaksatautiin (NAFLD), sydän- ja verisuonisairauksiin, haitallisen sisäelinten rasvan kertymiseen tai jopa syöpään. Normaali tai optimaalinen insuliiniherkkyys liittyy yleensä parempaan terveyteen ja aineenvaihduntaan.
///